April 1, 2014 — AccessClosure Inc. commercially launched its Mynx Ace vascular closure device, a safe and secure vascular closure product that provides consistent results with a new, easy-to-use deployment system to seal femoral artery access sites. [1] The device joins the pioneering line of Mynx extravascular products that help care teams reduce time to hemostasis and ambulation in patients who have undergone diagnostic or interventional endovascular procedures. The commercial launch was announced as part of the annual meeting of the American College of Cardiology.
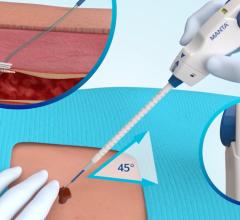
Mynx closure devices are designed for patient comfort by providing gentle vascular closure without the use of cinching, sutures, or metal implants to enhance patient satisfaction and keep physicians on the leading edge of patient care. [2] With Mynx Ace, physicians can consistently close femoral artery access sites through a simple, three-step deployment system. The Mynx Ace system uses AccessClosure’s proprietary Grip Technology, a major advancement in sealant technology. Grip technology employs an extravascular sealant that actively adheres to the artery for safe and secure mechanical closure and dissolves within 30 days, leaving nothing behind in the healed vessel.
“After completing over 50 cases with Mynx Ace, I have found the system provides consistent results while offering the safety, security and patient-friendly advancements I have come to trust in Mynx products” said Rajesh Dave, M.D., a cardiologist from Holy Spirit Hospital in Camp Hill, PA. “The advancements have made Mynx Ace a preferred closure device in my practice.”
Mynx Ace can be used with patients who have undergone diagnostic or interventional endovascular procedures utilizing a 5 French, 6 French or 7 French procedural sheath. It is estimated that more than 2.1 million of these procedures are conducted each year in the United States.
For more information: www.accessclosure.com
References:
1. As compared to earlier generations of Mynx closure devices. Test data on file at AccessClosure.
2. Fargen KM, Hoh Bl, Mocco J. J NeuroIntervent Surg (2011).


 October 07, 2025
October 07, 2025