Dr. Jeff Healey is seen implanting a subcutaneous defibrillator in a patient at the Electrophysiology Lab. Image credit: Owen Thomas, Hamilton Health Sciences.
May 2, 2022 – High-risk patients who need defibrillators to prevent cardiac arrest can experience fewer complications with a type of device implanted under the skin, a Canadian study has found.
Traditional defibrillators, while highly effective, involve placing a wire through a vein, into the chest and into the heart itself. The wires, known as ‘leads,’ in the traditional defibrillator - called a tranvenous ICD (TV-ICD) - can cause complications including perforations in the heart muscle or lungs and blood clotting in veins.
A study, conducted by researchers at Population Health Research Institute (PHRI) has demonstrated that a new type of cardiac defibrillator called a subcutaneous ICD (S-ICD) reduced patient complications by more than 90 percent, compared to the TV-ICD.
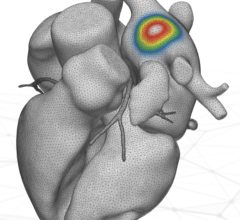
The S-ICD, implanted under the skin just below the patient’s armpit, does not involve any placement of leads into the heart or blood vessels. Instead, the S-ICD has a lead that runs under the skin, alongside the breastbone.
“The S-ICD greatly reduces perioperative, lead-related complications without significantly compromising ICD performance,” says Jeff Healey, a senior scientist at PHRI, a research institute of McMaster University and Hamilton Health Sciences (HHS).
“The S-ICD is now an attractive alternative to the TV-ICD, particularly in patients at increased risk for lead-related complications," adds Healey, a professor of cardiology at McMaster, and an electrophysiologist at HHS.
Healey presented the study’s results at Heart Rhythm 2022 in San Francisco.
The study involved 544 eligible patients (one-quarter females) with average age of 49, at 14 clinical centres in Canada.
They were electrocardiographically screened; 251 patients were randomized to S-ICD and 252 patients to TV-ICD. They were followed up for an average of 2.5 years to this point; follow-up is ongoing for the study.
Younger patients are usually under-represented in ICD trials,” says Healey. “However, our study included ICD-eligible patients 18 to 60 years old who had a cardiogenetic syndrome or were at high risk for lead-related complications.”
He added: "Canada has a strong history of ICD clinical trials and registries of patients with inherited heart rhythm disorders.”
Funding for the study was provided by Boston Scientific.


 July 30, 2024
July 30, 2024