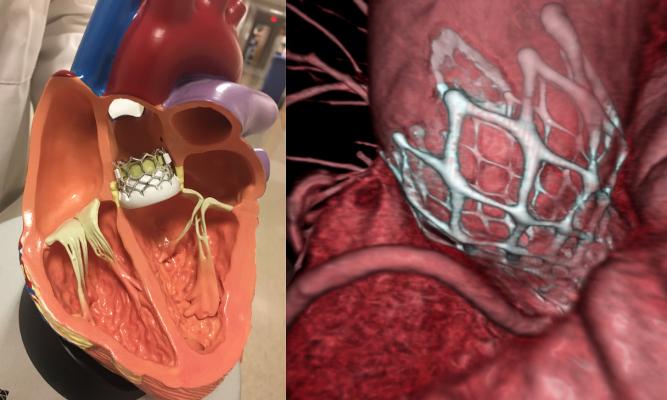
The two FDA-clear transcatheter aortic valve replacement (TAVR) valves on the market, the Edwards Lifesciences Sapien 3 (left) and the Medtronic CoreValve (right).
April 30, 2021 – An analysis of growth patterns in transcatheter aortic valve replacement (TAVR) programs across United States hospitals is being presented as late-breaking clinical science at the Society for Cardiovascular Angiography and Interventions (SCAI) 2021 Virtual Scientific Sessions. The findings indicate that TAVR structural heart programs are predominately located in metropolitan areas serving patients with higher socioeconomic status, potentially contributing to the disparities in cardiac care.
“TAVR has the potential to be an innovative and effective treatment option for heart valve patients, but can only work to its full potential if all patients have access to it. Our study results show a gap, and as clinicians, we know that these inequities can unfortunately translate into differing outcomes,” said Ashwin Nathan M.D., fellow, cardiovascular medicine, Hospital of the University of Pennsylvania, who presented the study. “While this is just one example of health inequities, our hope is that these findings will activate a change in how we introduce high-tech solutions, so that all communities can access the care they need.”
TAVR is a minimally invasive procedure for patients in need of a valve repair or replacement and is an alternative to surgical aortic valve replacement (SAVR), a treatment option requiring open heart surgery. TAVR also provides eligible patients with quicker procedure times and a shorter recovery. Yet, despite the benefits of novel therapeutics such as TAVR, some patients are still referred to SAVR even if they are ideal candidates – prompting a deeper analysis of how the technology is disseminated in certain populations.
The study involved a cross-sectional analysis of Medicare claims data between Jan. 1, 2012, to Dec. 31, 2018. Linear regression models were used to compare socioeconomic characteristics of patients treated at hospitals that did and did not establish TAVR programs to determine the association between area-level markers of socioeconomic status and TAVR rates.
The findings reveal inequitable access to TAVR programs for non-metropolitan or lower income areas across the country. Between 2012 and 2018, 554 hospitals developed new TAVR programs including 543 (98%) in metropolitan areas, and 293 (52.9%) in metropolitan areas with pre-existing TAVR programs. Compared with hospitals that did not start TAVR programs, hospitals that did start TAVR programs treated patients with higher median household incomes (difference $1,305, 95% CI $134 to $12,477, p=0.03). Furthermore, TAVR rates per 100,000 Medicare beneficiaries were higher in areas with higher median income, despite adjusting for age and clinical comorbidities.
The authors also acknowledge that increasing access to TAVR and structural heart programs will require foresight into how clinical trials and approval for procedures and technologies at hospitals are distributed.
Find out more in the VIDEO: Socioeconomic and Geographic Access to TAVR Programs is Limited — Interview with Ashwin Nathan M.D.
Find more news from the SCAI 2021 virtual meeting
Related Structural Heart Content:
Advice For Hospitals Starting a Structural Heart Program
BLOG: Creating a Structural Heart Program is an Investment in the Future of the Hospital
VIDEO: Advice For Hospitals Starting a Structural Heart Program — Interview with John Carroll, M.D.
Interventional Imagers: The Conductors of the Heart Team Orchestra


 November 14, 2025
November 14, 2025