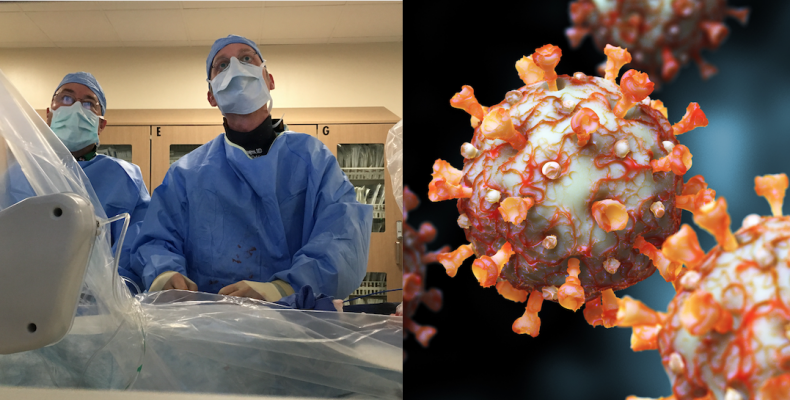
April 22, 2020 — The Society for Cardiovascular Angiography and Interventions (SCAI), along with the American College of Cardiology (ACC) and American College of Emergency Physicians (ACEP) issued a consensus statement that provides recommendations for a systematic approach for the care of patients with an acute myocardial infarction (AMI) during the novel coronavirus (COVID-19, SARS-CoV-2) pandemic. The document is jointly published in Catheterization and Cardiovascular Interventions, the official journal of SCAI, and the Journal of the American College of Cardiology (JACC).[1,2]
According to recent studies, cardiovascular disease patients who develop COVID-19 have a higher risk of mortality. However, many patients in need of care for the management of various heart diseases may not be infected with this coronavirus. The document identifies several challenges in providing recommendations for ST-elevation myocartdial infarction (STEMI) care during the COVID-19 epidemic. These include:
• Cardiovascular manifestations in the COVID-19 patient are complex and variable.
• The prevalence of COVID-19 in U.S. populations remains unknown.
• Personal protection equipment (PPE) is not uniformly available.
“During the COVID-19 pandemic we wanted to ensure that patients continue to benefit from the tremendous advances made in the care of patients with cardiovascular disease over the past three decades,” said Ehtisham Mahmud, M.D., FSCAI, SCAI president and lead author of the writing group. “Primary percutaneous coronary intervention (PCI) is the standard of care for STEMI patients, and in this document, we outline an approach to providing that therapy at PCI-capable hospitals while also ensuring health care worker safety with appropriate PPE.”
He said all STEMI patients should wear at least a surgical mask and all staff should wear N95 facemasks to limit contact with any aerosolized virus.
“When we talk about PPE, it has been a dynamic, rapidly changing environment, and the recommendations have been convoluted because of the supply chain issues,” Mahmud explained. He said the new guidelines say full PPE should be worn in the cath lab as a precaution to keep staff safe.
In cases where PPE is limited or not available, fibrinolysis can be used as a substitute therapy, according to the new guidelines.
If patients who can be stabilized should have PCI postponed if it is not an emergency
“The patients we recommend to delay eight weeks or so are the ones where they are stable enough where there is no significant risk of morbidity or mortality, everyone else should be treated on current best practices,” Mahmud said.
He also recommeds using a dedicated lab to treat COVID patients. “We have one cath lab that is dedicated for use with patients who are known COVID positive or high probably of having COVID-19, that cath lab is cleared out of all equipment and supplies and we wear full PPE," he explained.
The writing group recommends informing the public that exposure to the virus can be minimized, that patients continue to call the emergency medical services (EMS) when presenting with acute heart attack symptoms, and patients will be treated with primary PCI when indicated.
Fibrinolysis at referral hospitals without cath labs is appropriate with a plan of care for rescue or pharmacoinvasive PCI. The document also provides strategies for maximizing the safety of medical personnel with appropriate use of PPE and masking patients.
The document was summarized in key takeway points by Debabrata Mukherjee, M.D. on ACC's website:
1. Two point-of-care assays have recently received U.S. Food and Drug Administration (FDA) approval for rapidly making the diagnosis of COVID-19. As these tests become widely available, they should be routinely implemented in all STEMI patients to better characterize patient diagnosis and risk, optimize the treatment plan for a given patient (for AMI and or COVID-19), and guide appropriate placement within the hospital, including a dedicated cardiac catheterization laboratory (CCL) and post-procedure unit.
2. Adequate PPE is needed for all healthcare workers in the emergency medical service (EMS), transfer hospitals, PCI emergency department (ED), and the CCL team is critical. At this time, all patients requiring emergent activation of the CCL should be treated as COVID-19 possible. Given the potential risk of aerosol generation during all emergency AMI procedures, this writing group recommends PPE with aerosolization protection (including gowns, gloves, full face mask, and an N95 respiratory mask) for the entire CCL staff during PCI for all AMI patients during this COVID-19 pandemic.
3. Primary PCI is the standard of care for patients presenting to centers with cath labs (within 90 minutes of first medical contact). This should remain the standard of care for STEMI patients during the COVID-19 pandemic with some important caveats.
4. Each primary PCI center will need to monitor the ability to provide timely primary PCI based on staff and PPE availability, need for additional testing, as well as a designated CCL, which will require terminal cleaning after each procedure.
5. In the absence of these resources, a fibrinolysis first approach should be considered.
6. Additional time to establish an AMI diagnosis may be indicated (in some cases this may include echocardiography to assess for wall motion), and/or for COVID-19 status assessment and potential treatment (such as respiratory support). For these reasons, during the COVID-19 pandemic there might be longer door-to-balloon (D2B) times.
7. Due to the logistical issues and time delays secondary to diagnostic uncertainty of STEMI with COVID-19, direct transport of the patient to the CCL is not felt to be prudent at this time. The document recommend initial assessment of all STEMI patients in the ED during the COVID-19 pandemic to ensure the correct diagnosis and care plan. The attending interventional cardiologist should be notified, but without activation of the entire STEMI team until the plan for CCL activation is confirmed.
8. This document notes that not all COVID-19 patients with ST-elevation with/without an acute coronary occlusion will benefit from any reperfusion strategy or advanced mechanical support. In COVID-19 confirmed patients with severe pulmonary decompensation (adult respiratory distress syndrome) or pneumonia who are intubated in the intensive care unit and felt to have an excessively high mortality, consideration for compassionate medical care may be appropriate.
9. For non–ST-segment elevation acute coronary syndrome, COVID-19 positive or probable patients should be managed medically and only taken for urgent coronary angiography and possible PCI in the presence of high-risk clinical features (Global Registry of Acute Coronary Events [GRACE] score >140) or hemodynamic instability.
10. These recommendations will need to be adapted to each regional system’s PCI Center, STEMI referral hospitals, and EMS system and will need to be communicated clearly between cardiology and emergency medicine providers within each hospital. Systems need to recognize the competing principles of timely reperfusion, safe regional transport and treatment of potentially high-risk patients, while at the same time putting emphasis on the protection and safety of all healthcare personnel.
Other Impact of COVID-19 on Cardiology Content:
VIDEO: Impact of COVID-19 on the Interventional Cardiology Program at Henry Ford Hospital — Interview with William O'Neill, M.D.
VIDEO: 9 Cardiologists Share COVID-19 Takeaways From Across the U.S.
VIDEO: Multiple Cardiovascular Presentations of COVID-19 in New York — Interview with Justin Fried, M.D.
Image Gallery Showing Impact of the COVID-19 Pandemic
ACC COVID-19 Clinical Guidance For the Cardiovascular Care Team
VIDEO: COVID-19 Precautions for Cardiac Imaging — Interview with Stephen Bloom, M.D.
Reference:


 July 31, 2024
July 31, 2024 









