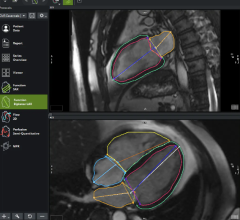
An example of advanced visualization and image navigation technologies from Philips to improve accuracy, speed and enable more complex transcatheter procedures.
A cardiovascular service line manager reader of DAIC recently e-mailed me and asked if I had a list of the top technologies that will likely change cardiology in the next few years. He wanted this information for a capital improvement planning for the next decade. I did not have this compilation handy, so I wrote the following list of 17 technology trends I feel will change how cardiology is practiced over the next 10 years, based on my industry observations. These items are not listed in any particular order of importance:
1. Expanding catheter-based interventions for all areas of the body. This will boost interventional radiology and cardiac cath lab volumes and lead to declines in open surgical procedures. As coronary interventions have plateaued, many of the new innovations in the coming years will be for heart failure and structural heart interventions. In the cardiac/vascular lab, new expansion areas will be in peripheral artery disease (PAD), critical limb ischemia (CLI), transcatheter valve repair and replacement technologies for all four heart valve positions, and interventional heart failure devices. Read the article "Predicting the Cath Lab of the Future."
2. Closer integration of computed tomography (CT) and echo imaging to provide better pre-procedural planning and peri-procedural guidance. Read the article "A Glimpse Into the Future of Cardiac Ultrasound."
3. Analytics software, combined with artificial intelligence, will see rapid uptake to look at big data across healthcare systems. This will enable new ways to manage healthcare, including identification of bottlenecks and inefficiencies within departments or processes. Analysis of big data will also enable population health initiatives to identify high-risk patients for screening programs and proactive outreach for checkup appointments. This can also help assess the readmission or infection risks a specific patient likely poses to help target limited hospital resources. Big data also offers a new way to conduct retrospective clinical studies. This might include analysis of the best protocols for treating patient subgroups that have a specific mix of various diseases. Or, it can highlight long-term outcomes or late complications for patients who are prescribed specific drugs or who received specific implantable devices. Read the article "Understanding How Big Data Will Change Healthcare."
4. We will see greater efforts and several new technologies to reduce radiation dose in both CT and cath lab angiography imaging systems. This includes increasing use of ultrasound and transesophageal echo (TEE) during procedures to cut or eliminate use of angiographic X-ray. There also will be increased use of 3-D navigation aids using 3-D echo, pre-procedural CT or rotational angiography imaging to reduce procedure times. A handful of centers also will build out interventional magnetic resonance imaging (MRI) suites to eliminate radiation entirely for long procedures, such as electrophysiology (EP) ablations.
5. There will be greater emphasis on reducing staff radiation dose and related orthopedic problems due to wearing heavy lead aprons all day. This includes adopting new technologies in the lab to better protect staff, including real-time dose monitoring systems, use of new, very light-weight aprons, and possibly robotics to remove the physician from the radiation field.
6. I predict wide adoption of virtual fractional flow reserve (FFR) technologies in the next decade if computer processing times can be reduced to minutes rather than hours. Current FFR combined with noninvasive CT angiography (FFR-CT) and advances like CT perfusion imaging will likely eliminate the need for nuclear myocardial perfusion imaging. In the cath lab, tableside FFR-angio now in development may eventually replace the need for the current gold standard of catheter-based FFR.
7. Transcatheter aortic valve replacement (TAVR) will likely replace the majority of open-heart surgical valve replacements in select patient populations. If clinical trial data continues the very positive trends for TAVR, it will gain more procedural volume than surgical valve replacements. It is a very good possibility this trend will be duplicated in transcatheter mitral and tricuspid valve repair and replacement technologies in the next few years.
8. Catheter ablation for atrial fibrillation will greatly improve from 60 percent procedural success rates to 80-90 percent in the coming years with the use of more accurate electro-anatomical mapping systems and improved ablation catheter technologies that reduce intra-operator variability. Both of these technologies are also helping reduce the time it takes to map and treat patients, which will allow for greater patient throughput and higher volumes in the EP lab. Improved accuracy and more complete abations also will reduce the number of repeat procedures. Watch the VIDEO "Current State of Atrial Fibrillation Ablation Technologies."
9. EP implantable devices will become much smaller and wireless. This will enable catheter-based implant procedures, eliminating need for surgical pockets and venous leads for pacemakers. These technologies also will reduce the number of leads required for ICDs. Watch the VIDEO "Current State of Leadless Pacemaker Technology."
10. All EP device followup and 24-7 monitoring will be conducted via the web through remote monitoring. Artificial intelligence will be used to help track patient data and identify patients who need office follow-up, device reprogramming and other issues requiring human interventions.
11. Simple, small wearable patient monitors will largely replace traditional Holter monitors. Consumer-grade patient monitors may offer new data to monitor patient health, including watching if a patient's health is declining or improving based on activity due to lifestyle changes, new drugs, etc. This data will need to be accessible for review and storage in patient electronic medical records. This may be automated as part of the larger trend of the Internet of things (IoT), and artificial intelligence will likely play a role in monitoring this data and alerting providers and patients of closely monitored, higher-risk patients. Read the article "How Smartphones and Apps May Change the Face of Healthcare."
12. Related to above is wearable or implantable technology that will also play a big role in better monitoring heart failure patients to prevent hospitalizations or readmissions.
13. However, with the new wireless connectivity of wearables and implantable devices, a new factor physicians may need to discuss with patients is cybersecurity risk. The U.S. Food and Drug Administration (FDA) is taking this very seriously and is working on new rules to better regulate cybersecurity management of these devices. Cybersecurity issues will also increase across healthcare with the further digitization of the industry and patient data. Read more on medical device cybersecurity.
14. There is a trend toward the "Uberization" of healthcare, where traditional office hours and care models will rapidly change to better match the digital interface and delivery of service models pioneered by Amazon, Uber and others. Like Amazon and Facebook, consumers today expect immediate results and access to their patient data, images, labs, etc. They do not want to wait a week for a radiology or lab report, or have to take time off work for a blood draw, imaging or to review test results with a nurse. Digital patient portals that integrate into the electronic medical record (EMR) and other reporting systems like the cardiovascular information system (CVIS), radiology picture archiving and communication systems (PACS) and laboratory reporting systems will play a key role in patient satisfaction. Telemedicine and patients using their own smartphone diagnostic tools will also likely play a big role in this in the future. This will start with medical care kiosks and move to web-based care for better provider access after normal business hours, weekends and late at night. Read about the Uberization of healthcare.
15. Across cardiac imaging, there will be greater use of 3-D advanced visualization. This includes fully automated reconstructions to improve efficiency and increase 3-D usage. This and other advanced visualization tools and image analysis will be immediately available at all staff workstations, not just dedicated computers. Some of this imaging capability will also be available for patients via their patient portals, and referring physicians via remote image viewing systems integrated with the EMR, PACS and/or CVIS. Advanced visualization in really complex cases will see a rapid increase in 3-D printed models from medical images. Holographic and true 3-D imaging will also see increasing use in radiology, cardiology and other specialities to better understand complex anatomy and for procedural planning.
16. CVIS, PACS and all other clinical data systems will be upgraded to systems that easily interface into enterprise-wide EMR systems. Some will be based around the hospital system's EMR as the main digital data access point. Others will be based around a vendor-neutral archive (VNA) that provides enterprise-wide access to the data using content management software to sort the data from all clinical systems and the EMR. Information technology (IT) departments will have a much greater say over what IT reporting systems are purchased and how departments and hospitals are wired, and will be the overall agents to interconnect all departments together into unified, enterprise systems. Read more on enterprise imaging.
17. Healthcare reforms to convert the current fee-for-service model to a fee-for-value model will continue because the payment system is inefficient, costly and is not sustainable for Medicare. While the pace of these reforms is slowing because of Trump administration policies, there is still a need to contain costs over the long term. Among these reforms will be movements toward bundled payments and the adoption of clinical decision support (CDS) software to determine if an order is appropriate for the specific patient. Both of these reforms were slated for 2017, but are now in question. The CDS for cardiac imaging (CT, MRI and nuclear) component is now pushed back to start in January 2018. Read about the CMS proposed CDS requirements. The goal for both of these reforms is to reduce costs by making hospitals look at ways to reduce their use of testing and become more efficient to enable profitability under bundled payments. The CDS component is designed to double check orders to ensure they are appropriate according to the standards of care set in guidelines by various cardiac and imaging societies. This includes imaging, procedures, drugs, etc. The systems are supposed to red flag any orders that do not match appropriate use guidelines, match previous orders already entered to reduce duplication, or highlight procedures, drugs etc. that may cause harm to a patient based on their specific data. These systems will likely incorporate an artificial intelligence component (such as IBM Watson). Read more about artificial intelligence in healthcare.
Related Trends in Cardiovascular Technologies:
8 Cardiovascular Technologies to Watch in 2020
Cleveland Clinic Unveils Top 10 Medical Innovations for 2020
A 40,000 Foot View of Trends in Cardiology
VIDEO: Editor's Choice of Future Healthcare Technologies at HIMSS 2015
Cardiovascular Advances to Watch in the Next Decade
Four Medical Technology Innovations We Might See in the Very Near Future based on MD Buyline's research.
I am always interested in readers' thoughts on new technologies and what they feel will be game-changers in the next decade. Feel free to drop me your thoughts at [email protected]



 November 14, 2025
November 14, 2025