The heart team approach was first used on a large scale in the CoreValve and Sapien TAVR trials and helped lead to excellent outcomes in high-risk patients.
In the current era of healthcare reform and the push toward evidence-based medicine to both lower costs and improve patient outcomes, the heart team approach to cardiac care has gained momentum. This is especially true in the area of structural heart intervention, where the concept was pioneered during the CoreValve and Sapien transcatheter aortic valve replacement (TAVR) trials. However, the heart team approach is also expanding to other types of structural heart intervention and in treating patients with complex coronary disease.
One thing that is evident is that teamwork and cohesion between the heart team members is just as important in cardiology as it is for a sports team on the field. Teams that work well together are successful, and those that do not communicate well will not be as effective.
Tenet Florida Heart and Vascular Network in South Florida has built a very successful structural heart and hybrid operating room (OR) program based on the heart team approach. At the 2016 Transcatheter Cardiovascular Therapeutics (TCT) conference, the heart team approach was a topic discussed in sessions by Brijeshwar Maini, M.D., FACC, interventional cardiologist, regional medical director of transcatheter therapies, and Brian Bethea, M.D., cardiac surgeon, regional medical director of cardiovascular surgery, both from Tenet Florida, Delray Beach.
The approach of using a structural heart or hybrid OR team enables patients to have a one-stop shop where they can get multiple issues taken care of by one set of specialists working together. This is especially important for more complex patients with multiple co-morbidities.
“That is the ultimate goal, to do everything we do from a cardiac surgery standpoint, but with a catheter,” Bethea said. “If we can treat the entire spectrum of pathology that these patients present with, then it will only lead to better outcomes, lower costs and less readmissions, and that is where the bundled payments are going.”
Watch a VIDEO interview with Maini and Bethea at TCT 2016
Building the Team
“We are best friends, we probably spend about 90 percent of our days together on the phone or in person,” Bethea said. “When you get the right heart team in place the communication is constant, and it needs to be for the best outcomes for your patients, and also for your program to be healthy. We involve our entire team and we prefer high performers without egos, those are the types of people we like to work with.”
Maini agreed. “Brian hit the nail on the head, we need to leave our egos behind, outside the door when we come in. We are all accomplished people in our own rights, and we were not trained to work the way we are working right now. So this is a learning experience for us,” he explained. This is a key element that is very important for centers just starting their structural heart or hybrid OR programs, he said. They need to be flexible and everyone needs to learn from each other and train across specialty lines.
“It is not just the collaboration between CT [computed tomography], surgery and interventional cardiology. It is truly a multi-specialty team,” Maini said. “You need your radiologists, you need your echocardiography, you need your valve clinic people, and so on. Even sometimes people in other areas like nephrology, because a lot of these patients also have renal issues, so they need to be a part of the team too and they need to understand what we will be doing to the patient. It might also include anesthesiology. So in the end, everyone needs to become part of this big happy family.”
The team is headed by the surgeon and the interventional cardiologist, but all the other team members contribute important pieces to the care and final outcomes with any patient.
“Another thing I feel is very important is that people need to understand the rigors of the other specialties,” Maini said. “Interventionists need to understand what the surgeons' issues are, and what is it that they can and can’t do. They cannot fix everything and we cannot fix everything, but as a team we can work together to decide what is the best option for the patient.”
Be on the Same Page
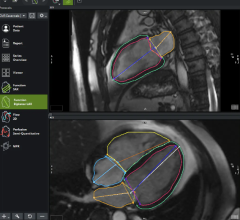
One of the common issues with new heart teams, or new members joining an existing team, is they all approach a problem from a different perspective that other team members may not understand. This includes use of different terms for the same thing, or different perspective on where something is located in the anatomy when trying to explain it during procedural guidance. This is especially true then looking at live echocardiography or transesophageal echo (TEE). Echocardiographers are limited by their imaging windows between the ribs and use standard views common in echo that are not used in angiography or CT, which are more familiar to interventionists and surgeons. This mainly includes viewing the heart in an upside-down position, but also includes creation of 3-D TEE views inside the heart that are not commonly seen during open heart surgery, such as looking at valves from a transapical position. This is why it is important to have open communication and be willing to ask questions or be willing to flip images around to a different position so the rest of the team is clear on what they are looking at.
“You need to be on the same page,” Maini said. “If you have an echocardiographer who is working with you, they need to be in sync with you. They cannot be out of sync with you, because otherwise it is no longer a team effort. They need to be in the procedure with you, not just be a surrogate showing you a couple of images.”
One of the things Bethea and Maini suggest doing on a team is change positions for who is lead on cases, so both the surgeon and interventionist can get used to working with a new device and understand what is needed. This helps make both operators more well rounded and they can anticipate what the lead operator will need or offer advice, especially when a procedure is not working or the patient has unanticipated issues.
“We have all been in situations where things are not going so well, we are all struggling and we are not getting the desired effect of what we initially planned, and it is a good idea when the other person is telling you that maybe it is time to stop,” Maini said. “It makes that decision process a lot easier, versus you as the operator having to make that decision to stop alone. Sometimes it is very difficult to do that, because you are so deep into the procedure at that point of time and you are not thinking that you should take a step back and take a deep breath. That to me personally, working side-by-side, is one of the biggest merits of a team that works with one another.” Maini said there are some heart teams in name only that do not work well together. “If they are really not working with one another and do not have that camaraderie, then that dialogue does not happen,” he explained.
Read the article “Requirements for Interventional Echocardiographers.”
Watch the video “What is Required for Interventional Echo - Discussion With Rebecca Hahn, M.D.”
Cats and Dogs Working Together for a Common Goal
In the past, there was intense competition between interventionists and surgeons. However, the heart team approach has enabled both sides to work together to determine what is the best approach for a patient, be it surgical or interventional. In the hybrid OR, it may be a mix of both, or a group decision based on what guidelines and current clinical trial data show as the best course of action.
Ten years ago, Maini said he never thought he would be working as part of a close-knit team with a cardiac surgeon. “This is a big cultural shift for all of us, and I think a cultural shift for the better,” he explained. “We are taking care of much sicker people than we were 10 years ago and we are getting better outcomes.”
He pointed to the great clinical outcomes from the CoreValve and Sapien TAVR trials in treating very sick patients who were considered too high a risk for surgical valve replacement. He said the excellent results in those trials were a direct result of interventionists and surgeons working side-by-side.
“There is no doubt in my mind that one person can do these procedures from a technical standpoint, but as I talk to the patients in the clinic I say, ‘You get the best of both worlds, you are getting a two for one,’ and who does not like a good value deal,” Bethea said.
This philosophy largely reflects the changes that have taken place at TCT over the past decade, where there are now whole tracts for cardiac surgeons.
“In the days gone by, surgeons were a rarity at TCT, it was an interventionist show," Maini said. "But today, it is as much a surgical meeting as it is an interventional meeting. And not just for TAVR, but also for coronary disease, high-risk PCI [percutaneous coronary intervention], chronic total occlusions, where heart teams are now discussing these cases. We all sit in a room now and ask what is better for this patient, surgery or PCI, and we let the chips fall where they may for the best outcome for the patient. If we do that well, at the end of the day we will have plenty of business for both sides. But, we cannot hold our patients close to our chests and not let go, because that is where we went wrong in the past. Being able to do what is best for the patient by using the technology that best fits that patient, not the operator, is really the Holy Grail.”
Patient Selection With the Heart Team
“Just because a patient has aortic stenoses, or mitral regurgitation or atrial fibrillation, it does not necessarily mean we should be treating them,” Maini said. “That is one of the things we have learned collectively. It is easier to determine this is a good patient population, but this is not a good patient population that we need to walk away from. That can only happen if the interventionist and surgeon are working together and learning from one another and each other’s past experiences."
A decade or more ago, Maini said surgeons would do the “eyeball test” to see if this is a patient they want to attempt treatment on, and they were burned with poor outcomes from some types of patients in the past, so they knew when it was a lost cause. He said interventionists would take these patients thinking they could fix everything with a catheter, but today they know better and realize their limits.
“The old adage is that a good surgeon is made because they have good judgment, and judgment comes from experience, and experience comes from making bad decisions,” Bethea explained.
He added that today, both surgeons and interventionists are working with new technologies and difficult pathologies. “So with a heart team it is nice because you have two people making that judgment instead of being out on an island by yourself,” Bethea said.
More and more, Bethea said cardiologists, surgeons and interventionists are being brought into the healthcare system as employees instead of being in private practice. He said a big advantage of this is being salaried, so it is more like an academic setting where you can pick and choose patients more carefully as the best candidates for procedures.
“You can say, ‘No, this is not the right candidate,’ because you are not worried about each patient being associated with your paycheck,” he explained. “And I think that frees you up to truly practice evidence-based medicine.“


 November 14, 2025
November 14, 2025