There has been a lot of conjecture that transcatheter aortic valve replacement (TAVR) may one day replace open-heart surgical aortic valve replacement (SAVR). However, after attending the American College of Cardiology (ACC) 2016 meeting, it is evident that change will come much sooner than anyone anticipated. “Wow” is really the key summary I can offer regarding the TAVR vs. SAVR data presented at ACC. Three key presentations were all positive for TAVR, showing it is at least equal or superior to surgery. This is not bad for a new technology with largely inexperienced operators being able to perform as well or better than cardiac surgeons with decades of experience.
The Partner 2A trial for the Sapien XT showed that the second-generation TAVR device was equal to surgery in intermediate-risk surgical patients. It was pointed out by experts in numerous ACC sessions that if the two techniques are equal, the minimally invasive method will usually win out as a new standard of care.
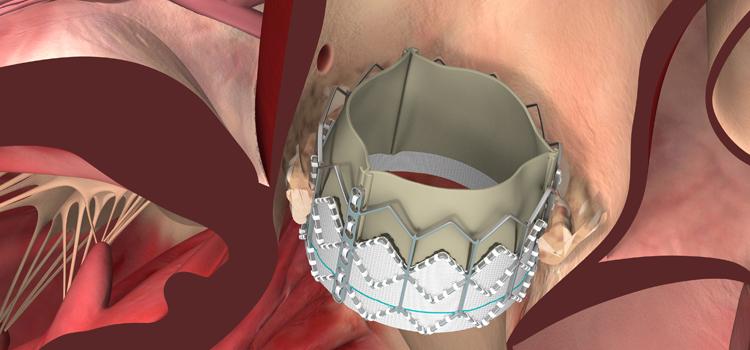
The improved Sapien 3 device replaced the XT toward the end of the Partner 2 trial. The valve has a fabric skirt that significantly reduces paravalvular leak, which was an issue with the earlier XT and the original versions of the Sapien. The PARTNER results were separated for the XT and Sapien 3 arms of the study. The data for Sapien 3 show it performed better than surgery in intermediate patients.
Watch a video interview with Vinod Thourani, M.D on the Sapien 3 beating surgery.
U.S. CoreValve pivotal trial results showed TAVR was better than surgery, and the three-year results presented at ACC show a continued positive trend. The lines between TAVR and surgery for all-cause mortality also continue to diverge in favor of TAVR.
Stoke rate have been high with TAVR compared to surgery in earlier trials, but that rate has dropped in recent trials presented at ACC.16 to now be equal with surgery.
Cardiothoracic surgeon Steven Bolling, M.D., University of Michigan, said TAVR is a brand new technology being implanted by new, inexperienced operators. But, within five years of the technology gaining U.S. market approval, it has beaten out the performance of very specialized, experienced surgeons. He noted that new interventional cardiology operators were able to show better patient outcomes with TAVR than his own surgical outcomes, and he has the experience of performing more than 5,000 surgical valve procedures. Bolling said if a test between two competing technologies shows them to be at least equal, the easiest one to use will always be the ultimate winner. He said there is little doubt in his mind that TAVR will become the standard of care in the next few years.
The three main questions standing in the way of full acceptance of TAVR as a new standard of care are: 1. How it performs in low-risk patients; 2. Durability; and 3. Its ability to gain reimbursement. The U.S. Food and Drug Administration (FDA) gave the green light earlier this year for low-risk patient trials for both the CoreValve and Sapien 3. The results of those trials in a couple years will be very highly anticipated. The long-term durability of TAVR valves will also be assessed in these patients over the next decade.
Long-term durability data has been hard to track in the extreme- and high-risk patients included in the early PARTNER and CoreValve trials due to high mortality rates. So, this data is expected from the intermediate- and low-risk patient studies, but this will require seven to 10 years of data before a clear picture of durability emerges.
Reimbursement is still an issue, especially with the average cost of TAVR being several thousand dollars more than surgery. However, the cost of the devices and of the procedures will go down as TAVR’s usage expands, the experts say, as with any new technology. The current cost-conscious healthcare environment will also likely embrace TAVR as the cost drops, especially as this minimally invasive technique increasingly becomes a same-day outpatient procedure.



 July 31, 2024
July 31, 2024 









