November 23, 2015 — A new 3-D computer modeling system may significantly improve a surgeon’s ability to select the best-sized donor heart for children receiving heart transplants, according to research presented at the American Heart Association’s Scientific Sessions 2015.
Transplant centers currently assess compatibility of a potential donor heart by comparing the donor weight to the recipient weight and then picking an upper and lower limit based on the size of the patient’s heart on chest X-ray. But the assessment is not precise and variations in size and volume can have a major effect on the recipient’s outcome.
While survival in pediatric heart transplantation have improved, there are still too few donors to meet the demand, so “it is critical to optimize the range of acceptable donors for each child,” said study author Jonathan Plasencia, B.S., a Ph.D. student at Arizona State University’s Image Processing Applications Lab in Tempe, Ariz.
“3-D reconstruction has tremendous potential to improve donor size matching,” he said. “We feel that we now have evidence that 3-D matching can improve selection and hope this will soon help transplant doctors, patients, and their parents make the best decision by taking some of the uncertainty out of this difficult situation.”
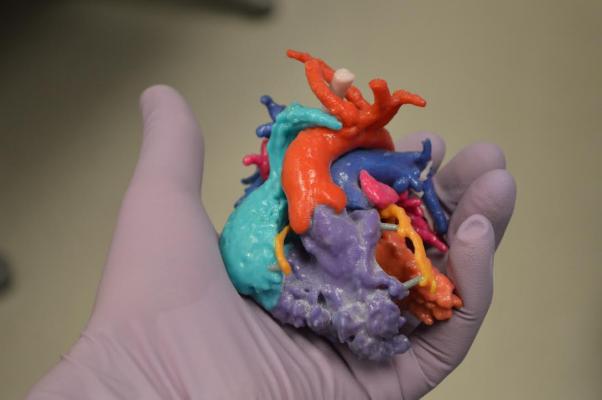
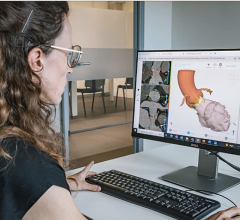
To develop the new 3-D system, the researchers created a novel library of healthy children’s 3-D reconstructed hearts using magnetic resonance imaging (MRI) and computed tomography (CT) images in children weighing up to 99 pounds. They then used the library to predict the best donor body weight to ensure the correct heart size needed for pediatric transplant recipients. Then they used before and after images from infants who had already received a heart transplant. When they compared the post-operative data from the real infants with the virtual transplant images, they found that the 3-D imaging system accurately identified an appropriate size heart.
“As the virtual library grows, the ability to accurately predict donor heart volumes will improve, and analyzing future transplant cases using 3-D matching will allow us to predict the true upper and lower limits of acceptable donor size,” he said. “This may allow more effective organ allocation on a national scale and minimize the number of otherwise acceptable organs that are ultimately discarded.”
Researchers suggested that one day transplant teams may be able to use the 3-D process to perform virtual transplants before an actual procedure to rapidly measure a donated heart to ensure a better fit and to reduce the risk of mismatching in pediatric transplants.
The 3-D process was a collaborative effort developed at the Arizona State University, along with researchers at Phoenix Children’s Hospital and St. Joseph’s Hospital and Medical Center, also in Phoenix. The team was overseen by Steven D. Zangwill, M.D., medical director of heart transplant and heart failure at Phoenix Children’s Hospital.
Although not yet to the point of replacing size matching for transplants, the investigators are encouraged by what they have found and have already implemented the techniques to supplement standard of care at Phoenix Children’s Hospital, Plasencia said.
The big question is how long it will take to further test the technique and move it into actual use.
“We are hoping that over the course of the next year, we will have a better sense of its validity in a prospective study,” Plasencia said.
Co-authors are Justin Ryan, Ph.D..; Jacob Lindquist, B.S.; Susan Sajadi, B.S. Micheal Van Auker, Ph.D.; Randy Richardson, M.D.; Erik Ellsworth, M.D.; Susan Park, C.P.N.P.; Robyn Augustyn, B.S.; Richard Southard, M.D.; John Nigro, M.D.; Stephen Pophal, M.D.; David Frakes, Ph.D. and Steven Zangwill, M.D. Author disclosures are on the manuscript.
The study was not funded by any outside sources.
For more information: www.scientificsessions.org

 October 21, 2024
October 21, 2024 









