August 28, 2015 — Cardiologists from Children’s Hospital Los Angeles successfully implanted a Melody Transcatheter Pulmonary Valve in child actor Max Page, the boy who made headlines playing mini Darth Vader in a 2011 Super Bowl ad for Volkswagen.
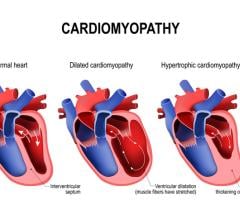
Page, now 10, suffers from a congenital heart disease, tetralogy of Fallot, and he was recently diagnosed with conduit stenosis, a condition that was restricting blood flow from the right ventricle of his heart into his lungs due to a narrowing of the pulmonary valve, which had been surgically implanted in 2012.
“We had a great result; Max has a new heart valve, and we hope it will last a long time,” says pediatric interventional cardiologist Frank Ing, co-director of CHLA’s Heart Institute and leader of the cardiology team that performed the three-hour procedure July 30. “His pulmonary valve function has been restored and we avoided open-heart surgery.” The stenosis, Ing explained, had been restricting the flow of blood into his lungs and was also leaking blood back into his heart. But tests performed by Children’s Hospital the morning after the procedure showed significant improvement in Max’s heart function, Ing said.
On Tuesday, Sept. 1, Max will have a procedure at Children’s Hospital Los Angeles to replace his pacemaker pulse generator. It will be his second operation in 34 days. This device is implanted in the abdominal wall and keeps track of Max’s heart rhythm through electrodes sewn to the heart. It stimulates the heart muscle with an electrical impulse to maintain the appropriate heart rate for whatever activity Max is doing at the time. “Since the pulse generator runs on batteries, it needs to be replaced at periodic intervals, usually every five to seven years,” explains cardiothoracic surgeon Winfield Wells.
After undergoing the Melody Valve procedure in July, Max was discharged from the hospital the very next day. “Max was a little sore, but he was able to walk, jump and move for Dr. Ing the morning after surgery,” said his mother Jennifer.
“I’m feeling good,” Max said just before his discharge, taking a practice golf swing in shorts and a polo shirt in his hospital room. Speaking beyond his years from his hospital room, he added, “The staff here is really great and the doctors are very happy.”
“It’s just amazing to think Max can receive a new heart valve and be out of the hospital in 24 hours,” said Max’s father Buck. “The last time we were here for open-heart surgery, he had a 10-inch chest scar and he was on morphine for three days. Now he is going home with a couple of Band-Aids and some Tylenol.”
Born with a congenital heart defect, Max had his first surgery at age 3 months. The Melody Valve procedure was his 10th operation, said Jennifer, explaining that Max first began complaining of fatigue and exhaustion earlier in the summer. “He just wasn’t his usual self,” she said of her son, who likes to play golf, guitar and act (he has recurring roles on the soap opera “The Young and the Restless” and the Disney Channel series “I Didn’t Do It”).
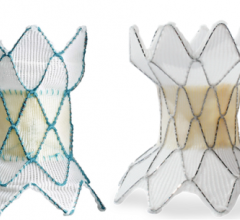
Ing said that an echocardiogram in mid-July indicated an inconsistency with the force that propels blood, called the gradient pressure, through Max’s pulmonary valve. During the procedure, Ing confirmed a high gradient across the narrowing caused by a thickened pulmonary valve, constricting blood flow. To open the valve, Ing first dilated a balloon inserted via a catheter running through blood vessels from Max’s thigh to the pulmonary valve. But this only partly improved the pressure gradient and the heart was still working too hard to pump blood into Max’s lungs. After consulting with CHLA cardiothoracic surgeon Vaughn A. Starnes, co-director of the Heart Institute, Ing moved on to the second option — inserting a Melody Valve inside the old pulmonary valve. First, his team ran a test inflation of the Melody Valve to make sure the new valve would not affect the function of the nearby coronary artery, which could trigger a heart attack on the table.
Using specialized high-resolution X-ray imaging to guide his catheter back into the existing pulmonary valve, Ing dilated the Melody device to the appropriate diameter to allow the blood to flow with consistent pressure between the heart and lungs. “We use a team approach at CHLA,” says Ing, a specialist in complex cardiac catheterization procedures. “We determined that by opening the pulmonary valve with the Melody Valve, this would widen the existing narrowing to allow the heart to work less hard. It’s like clearing an accident on a freeway to open up all the lanes for traffic.”
The Melody was granted premarket approval this year by the U.S. Food and Drug Administration (FDA), but has been used in children as a federally designated humanitarian device intervention for several years. The primary benefit of the procedure in children is that it can increase considerably the time between surgeries, allowing children an opportunity to grow so cardiologists and surgeons can use adult-sized devices, reducing the need to replace them as young patients grow older. This less-invasive procedure also allows for both shorter hospital stays and recovery times for heart patients.
Had the Melody device not been a viable option, Max would have been scheduled for open-heart surgery to implant a new pulmonary valve. The hospital is currently fundraising to build a hybrid surgery suite that would allow CHLA cardiologists and surgeons to convert the room from a catheter lab to a surgery suite instantly, so physicians can collaborate on cases and patients can have complex catheter procedures and surgeries done on the same day. The Children’s Hospital Los Angeles Heart Ambassadors—co-chaired by Jennifer and Buck Page—has been leading the fundraising effort for two years.
“Had Max needed surgery again, it would have been better to do it at the same time,” Jennifer said. “But in the future, this hybrid surgery suite will be a tremendous benefit for all CHLA heart patients.”
In 2012, Max had his pulmonary valve replaced during a two-hour surgery at CHLA. While his physicians had hoped the pulmonary valve would last longer, many variables affect that outcome, such as how an individual’s body reacts to the new valve. “It’s possible that the growth of the tissue around Max’s pulmonary valve was affected by Max’s own body’s process of healing after his last surgery, ” Ing said. “There were places where the valve appeared thicker than I would have expected. But no one understands the cause or why it happens to one valve but not to another, or in different patients.”
The morning of the July procedure, Max waited with his family, fighting off hunger pains and playing video games on a mobile phone. “I’m feeling a little tense and nervous, but I know the doctors are going to do a good job,” he said. During the procedure, he kept a small Bible in a bag near his gurney as his family waited in the Heart Institute family lounge. Jennifer, Buck, Max’s brother Els and their maternal grandparents reminisced about Max’s previous visits to CHLA and said private prayers. Els rubbed his angel coin for good luck. “Els was a rock star and was determined not to eat until Max went in for surgery,” said Jennifer, who was impressed by her younger son’s multitasking. “When we got word that Max would need more than just a dilation of the valve, Els texted us, ‘Keep praying.’”
Max resumed most of his activities within days, though he remains restricted from playing contact sports over the next several months and will need periodic follow-up echocardiograms to monitor the new valve. “It never goes away,” Buck said. “Max will be dealing with this his entire life. It’s something he’s aware of, but he wants to experience life to the fullest and we want to make sure that he has that.”
For more information: CHLA.org


 March 31, 2025
March 31, 2025