May 7, 2014 — Women face greater limits on their lifestyle and have more severe symptoms as a result of peripheral artery disease (PAD), but minimally invasive procedures used to unclog arteries are just as successful as in men. The success of procedures, such as angioplasty or stent placement, in treating women with leg PAD was revealed in a Journal of the American College of Cardiology study.
The study provides a rare look at gender differences in PAD. PAD happens when fatty deposits build up in arteries outside the heart, usually the arteries supplying fresh oxygen and blood to the arms, legs and feet. About 8 million Americans have peripheral artery disease, but PAD awareness among men and women is strikingly low compared with other cardiovascular diseases like hypertension and heart attacks.
“We found that women had excellent outcomes compared to men, even though they were older and had more severe disease,” says senior study author P. Michael Grossman, M.D., an interventional cardiologist at the University of Michigan Frankel Cardiovascular Center and director of the cardiac catheterization laboratory at the Veterans Administration Ann Arbor Healthcare System.
Before treatment, women were at higher risk of amputation, and more likely to suffer from leg pain at rest or ulceration, called critical limb ischemia. Fewer women complained of leg discomfort, fatigue or cramping with activity known as claudication, according to the study.
“The reasons for differences in symptoms are unclear, and deserve further study. It does indicate that we need to be vigilant in asking women about leg discomfort and screening women for PAD,” says Grossman.
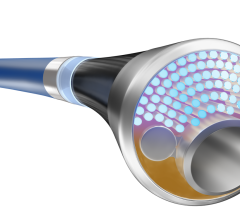
Researchers used Michigan’s Blue Cross Blue Shield of Michigan Cardiovascular Consortium PVI registry, which collected data from 16 Michigan hospitals about percutaneous peripheral vascular intervention. A total of 12,379 patients had lower extremity PVI from 2004 to 2009, and the overall procedural success rate of PVI was 79 percent for women compared to 81 percent for men. There was also no difference in heart attacks or strokes.
It was surprising, researchers say, to observe no gender-related differences in procedural success considering that women experienced more transfusions, vascular complications and embolisms. “The data suggests women may benefit to a greater degree with an invasive percutaneous strategy for the management of PAD, particularly if complications can be avoided,” says study author Elizabeth Jackson, M.D., cardiologist and director of the University of Michigan Women’s Heart Program.
According to the study, women were less likely than men to be prescribed cholesterol-lowering statins and antiplatelet therapy before the procedure. “We need to work together to ensure all patients with PAD are prescribed these medications, particularly women,” Jackson says.
Some patients need minimally invasive procedures to unclog arteries and restore blood flow, but lifestyle changes, such as quitting smoking, exercise and medications are known to slow or even reverse the symptoms of PAD.
For more information: www.med.umich.edu


 September 12, 2025
September 12, 2025