With respect to advances in cardiovascular care and treatment technology, most of today’s conversations center on how they impact and improve patient care, treatment costs and outcomes. Patients, after all, stand at the center of everything we do in healthcare. But let’s not forget the providers.
Patients do not have to be the only beneficiaries of technological innovation. Indeed, many technological hardware and software solutions are emerging to help cardiac care providers negotiate their way through a healthcare environment that’s increasingly competitive, cost-conscious and challenging.
Continuing Consolidation
One of the more significant challenges facing cardiology providers revolves around the aggressive consolidation of health systems, which is wreaking great upheaval on the day-to-day operations of many cardiology providers. Just 18 months ago, most U.S. cardiologists worked in private practice, contracting their services to hospitals and health systems. Today, most are, or are becoming, employees of healthcare delivery systems.
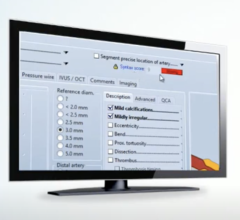
At the same time, these cardiologists and the systems they serve must contend with the continuing challenge of staying up-to-date on and leveraging new technology, such as optical coherence tomography (OCT) and new procedures including transcatheter aortic valve replacement (TAVR). Tools and techniques like these promise to revolutionize cardiac care and treatment.
Unfortunately, it is no longer as simple as just buying the latest technologies and plugging them into practice. In today’s changing environment, each new solution needs to be evaluated in terms of its impact on workflows and the ease of incorporating it into a system’s cardiovascular service line.
This presents challenges for both the cardiologists and the systems they are joining. As individual practices, most cardiologists worked with their own set of tools — one vendor solution for echocardiography, another for cardiac catheterization and so on. But now that they are becoming part of enterprises that have their own solutions, many cardiologists and interventionalists are being forced to change their workflows and adapt to using new tools that they may not be familiar with.
Change Management for People and Technology
The key lies in effective change management, with respect to both people and technology. Healthcare systems that take on the role of collaborator and build a solid plan to acquire and integrate new practices and technologies are likely to find that the process goes more smoothly. That means making individual cardiologists part of the discussion from very early on, in addition to integrating the cardiologists’ own tools and processes into the system wherever and whenever possible.
Acquisitions happen over time, and cardiologists should have an opportunity up front to talk about the tools they are using and how they might fit into the new system. From the health system’s side, it also helps to identify a physician champion and enable that person to help get buy-in from their colleagues.
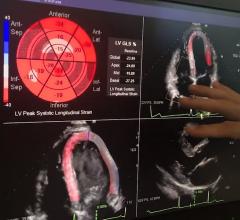
Technological innovations, particularly in regard to leveraging cardiology-specific tools integrated with the enterprise’s electronic medical record (EMR), are changing the landscape and making it easier for providers to streamline workflows and thrive in this new environment. One key, especially for healthcare systems in the process of acquiring cardiology practices, is to ensure that the infrastructure is in place to integrate these new technologies and to migrate all the images from disparate systems into a central depository, or vendor-neutral archive (VNA).
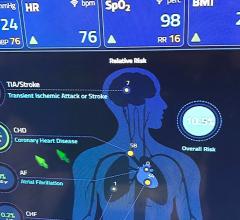
From a clinical perspective, there also is a lot going on with the integration of cardiovascular information systems (CVIS) and EMRs. One example is medication administration in the cardiac cath lab, which has always been something of a “black hole” to the EMR. Typically, when a patient comes down from the floor to the cath lab for a procedure, medications that are administered in the lab are documented in a hemodynamics system, but the EMR is completely unaware of them. This prevents staff on the floor from access to a complete picture of what treatments have been completed. Fortunately, today there are bidirectional, real-time interfaces that not only send the medications administered in the cath lab directly into the EMR, but can also alert the staff in the cath lab in real time of any medication allergies or drug-to-drug interactions that may exist. This both solves the long-standing clinical workflow problem, and more importantly results in significantly improved patient care.
Another example lies in image access and interoperability. With today’s focus on cost cutting, duplicative imaging studies are a prime target; solutions are available today to link all of a patient’s cardiac imaging studies directly within his or her electronic chart, making imaging consultations and referrals feedback much faster and more efficient.
Weeding Out the Tools From the Toys
With respect to the goal of creating a single, seamless and easily accessible patient record that includes data and images, there is no shortage of technology in today’s marketplace. The challenge is to separate the truly valuable and necessary tools from the whiz-bang “toys.”
The key is to ask the right questions. Not long ago, those were questions like, “how does your solution help me archive and manage my images?” and “what viewer features do you offer?” Today, the more relevant questions — and answers — center on integration:
• How comprehensive and scalable is your solution?
• Does your solution cover all the imaging specialties, from echo to cath to nuclear to non-invasive vascular and so on?
• Is your solution really good at echo and not as good with the other specialties?
• Does your solution easily scale up to accommodate acquisitions?
• How well does this solution integrate with my EMR?
• How is my EMR going to be image-enabled with this new solution?
Other questions should zero in on a solution’s reporting capabilities. KLAS recently issued a cardiology report for 2013 indicating that the biggest differentiator among CVIS solutions focuses on structured data clinical reporting. Buyers should be asking how easy structured reporting is for physicians to leverage with respect to a given solution, and how quickly that information can be returned to the referring physician.
Referrals are big money; doing a great job for referring physicians helps grow a cardiology business, and these are also some of the questions providers should be asking of any solution under serious consideration.
Let Usefulness Be Your Guide
Health systems and cardiology providers of all types and sizes are in the midst of transitioning to a new era in healthcare that replaces traditional care and treatment models with value-based models. The providers that will be most successful at making the transition will be those that ensure their solutions reflect their strategy going forward. Providers that are in a very acquisitive mode, for example, will make certain whatever solution they’re considering is going to scale appropriately. They’ll also ensure they get a VNA that hits all their specialties, and they’ll demand a common reporting engine so they can do their analytics across all the cardiology specialties.
Ultimately, the health systems and cardiologists with that motivation at the forefront — to make the most efficient use of their EMR in conjunction with their CVIS — and who make it less about acquiring the latest and greatest “toys,” are the ones that will be in place to win in the long run. These are the ones that will reap the greatest benefits of consolidated systems and data.
Best Practices for Succeeding in the New Era of Cardiac Care
Administration:
• Strategize. Build an overarching strategy or plan for your cardiology services.
• Collaborate. Identify and collaborate with your peers – health systems in the same market segment, employing a similar marketing strategy. Discuss what’s working and not working with them.
• Research. Study vendors and their offerings. Talk to your peers about them, as well. Find out what’s worked well and what’s worked poorly for them.
Clinicians:
• Be involved. Participate in the technology selection process and participate in the integration. This ensures that your voice will be heard and that you’ll be part of the solution.
• Collaborate. Like administrators, you should collaborate with your colleagues; talk to them about what solutions are proving most and least successful.
Editor’s note: Bob Schallhorn is vice president, imaging solutions, at Merge Healthcare. Merge provides EMR, PACS and CVIS solutions.



 November 06, 2025
November 06, 2025