May 13, 2013 — A new method of dynamic, personalized intravenous hydration significantly reduces the percentage of contrast-induced kidney injury from image-guided cardiovascular procedures, according to the results of the POSEIDON clinical trial presented as a late-breaking clinical trial at the SCAI 2013 Scientific Sessions.
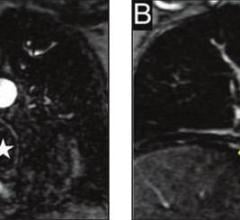
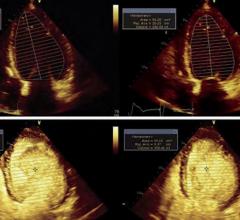
Interventional cardiologists are able to perform minimally invasive procedures, such as angioplasty and stenting, because of imaging technologies that allow them to see inside the heart and blood vessels without open surgery. Use of iodine-based angiography imaging contrast media is generally safe, but for some patients with drug sensitivities or compromised kidney function, a complication called contrast-induced nephropathy can result. To prevent this complication, most institutions deliver intravenous saline hydration, which until now has not been tailored to the individual patient. The POSEIDON trial compared this standard hydration method with a new model for intravenous hydration that measures a patient’s blood pressure to determine how much hydration to provide.
“Hydration is the cornerstone for preventing damage to the kidneys, yet fundamental gaps in our knowledge remain,” said Somjot S. Brar, M.D., MPH, interventional cardiologist, vascular specialist and vice chair of area research at Kaiser Permanente Los Angeles Medical Center in Los Angeles, Calif. “For example, there is little evidence to help guide rate and duration of hydration. The results from this trial provide a concrete framework for performing hydration.”
POSEIDON is the first randomized clinical trial to study personalized hydration based on an aspect of the patient’s own blood pressure. The trial enrolled 396 patients with a mean age of 71 and stable renal insufficiency who were undergoing coronary angiography or percutaneous coronary intervention. Prior to their procedure, patients were divided into two groups, either receiving standard hydration or hydration calculated based on a measurement of intra-cardiac pressure called left ventricular end-diastolic pressure (LVEDP). Both groups received hydration via saline IV throughout the procedure and for four hours afterward.
Approximately 7 percent of patients in the experimental group experienced contrast-induced nephropathy, versus approximately 16 percent of patients treated with standard hydration.
The cumulative rate of major adverse events, tracked over six months and registered as a composite of dialysis and other renal therapy, heart attack and death, was 68 percent lower in the group that received personalized hydration.
“Hemodynamically guided hydration significantly reduced the rates of both contrast-induced nephropathy and major adverse events,” said Brar. “This is the first contrast-induced nephropathy prevention study to show a major reduction in important clinical events. We believe these findings should impact clinical practice and will likely have important implications for patients at risk of contrast-induced nephropathy undergoing cardiac catheterization.”
To watch a video of this data presentation from the 2012 Transcatheter Cardiovascular Therapeutics (TCT) meeting.
Brar reports no conflicts of interest.
For more information: www.scai.org


 August 17, 2023
August 17, 2023