August 25, 2011 – Two articles in the Society of Interventional Radiology (SIR)'s flagship publication, the Journal of Vascular and Interventional Radiology, report on studies related to peripheral arterial disease (PAD), coinciding with the approach of September's National PAD Awareness Month.
In one study, researchers determined that Framingham Risk Score metrics (historically the gold standard in predicting 10-year cardiovascular risk) alone may not be enough to definitively say whether an individual may face a future cardiovascular event. The second study examined the success of a treatment option for what could be a serious complication of PAD. For more than a decade SIR has sponsored Legs For Life, a national screening program designed to detect peripheral arterial disease early, when lifestyle changes and medication could improve symptoms and possibly circumvent serious consequences.
"As these studies show, early detection and intervention is crucial to a good outcome. An integrated program like Legs For Life assists communities with early detection and management of peripheral arterial disease," said Sanjay Misra, M.D., FSIR, chair of SIR's PAD Service Line.
"The Society of Interventional Radiology's Legs For Life national screening program wants to make individuals aware of the existence of undetected health problems, help identify whether they have PAD and encourage them to seek follow-up with their primary care doctor and an interventional radiologist," said Misra, the interventional radiologist at the Mayo Clinic and Foundation for Medical Education and Research in Rochester, Minn. "The public — as well as the medical community — need to understand the importance of the diagnosis of PAD in terms of symptoms and, more importantly, in how a diagnosis of PAD brings added risk of heart attack, stroke and death."
An estimated 10 million people suffer from PAD — a common yet serious disease that is an indicator for heart attack (the leading cause of death in the United States) and stroke — and many with the disease may be unaware that they have it. PAD develops mostly as a result of atherosclerosis or hardening of the arteries, which occurs when cholesterol and scar tissue build up, forming plaque that narrows and clogs the arteries, slowing blood flow to the legs. Symptoms — such as leg pain while walking, numbness and tingling in the lower legs and feet, coldness in the lower legs and feet, or ulcers or sores on the legs or feet that don't heal — could be PAD warning signs. Risk factors such as smoking, diabetes, high blood pressure, high blood cholesterol and obesity are associated with increased risk of heart attack and are routinely monitored by doctors to identify at-risk patients. However, about two-thirds of coronary events occur in individuals not known to be at high risk and physicians know that often, by the time that heart problems are detected, atherosclerosis is usually quite advanced, having progressed for decades.
A common formula called the Framingham Risk Score is used to estimate the 10-year cardiovascular risk of an individual. "Traditional risk-scoring algorithms, such as the Framingham Risk Score, have low sensitivity for predicting risk of fatal or nonfatal cardiovascular events," said Rajoo Dhangana, M.D., of Bridgeport Hospital in Bridgeport, Conn., one of the authors of the study, "Prevalence of Abnormal Ankle Brachial Index Among Individuals With Low or Intermediate Framingham Risk Scores."
"Ankle brachial index, a noninvasive and simple screening test for peripheral arterial disease, compares blood pressure reading in the arm and ankle. This is shown to have potential to improve identification of individuals who are otherwise not considered to be at high risk for heart attacks," said Dhangana.
Screening programs such as SIR's Legs For Life often use an ankle brachial index (ABI) to determine how well the blood is flowing and if additional tests are needed. The ABI is a direct measure of fatty plaque buildup in leg arteries and an indirect gauge of plaque accumulations throughout the entire cardiovascular system. Because atherosclerosis is a systemic disease, women and men developing plaque in their legs are likely to have plaque building up in the carotid arteries, which can lead to stroke, or in the coronary arteries, heart attack, explained Dhangana.
"Evaluating the connection between peripheral arterial disease and heart disease is important, as an abnormal ankle brachial index is associated with a higher risk of cardiovascular disease and is considered a marker for coronary heart disease or its equivalent," Dhangana said.
In the study, Dhangana and fellow researchers examined the Framingham Risk Score variables from 822 participants (women, 69.7 percent; non-Hispanic white, 89.7 percent) without known cardiovascular disease or diabetes. The participants' Framingham Risk Scores alone showed 463 (56.3 percent) were deemed to be at low risk; 212 (25.8 percent) at intermediate risk; and 147 (17.9 percent) were at high risk. When researchers examined the ABI scores of these three groups during evaluations at 23 Legs For Life sites across the United States, said Dhangana, abnormal ABI readings were recorded in 12.3 percent of those deemed low risk and in 12.2 percent of those categorized as intermediate risk, using Framingham scores alone.
"By itself, Framingham assessment is not 100 percent accurate in predicting a future coronary event," said Dhangana. "Ankle brachial index testing should be an important part of the screening process because even those identified as low risk with Framingham metrics could face coronary heart disease in the future," he said.
Early detection of PAD is important because when individuals are at significantly increased risk, preventive measures can be taken. Since the leg pain caused by PAD is one indicator for heart attack and stroke, interventional radiologists can partner with primary care doctors, who may not be aware of or be able to administer noninvasive tests like the ABI in managing patients' vascular disease. When PAD is diagnosed, physicians may first recommend lifestyle changes and medical intervention, all of which can be started before costlier and more intensive interventions are needed. If necessary, interventional radiologists can perform minimally invasive treatments such as angioplasty and/or stenting to open a blocked artery in the leg and restore blood flow.
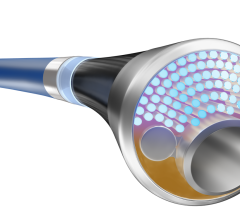
Researchers noted that sometimes, when lifestyle changes to combat PAD are unsuccessful in stemming the disease's progression, dangerous aorto-iliac lesions — wounds on or near pelvic arteries — may develop. In "Bifurcated Endograft in Aorto-iliac Type C and D Lesions: Long-term Results," Tobias Zander, M.D., an interventional radiologist with the department of endovascular therapy, Hospiten Rambla, Tenerife, Spain, examined the use of a bifurcated prosthesis as an alternative to bypass surgery on these types of lesions.
"In this study, a type of prosthesis that is normally used to treat aneurysm of the lower aorta, but has also been employed successfully for the treatment of these lesions, was placed in 14 patients with no related amputation or death," said Zander. "Patients were followed up for an average of 62 months. Occlusion was noted in only two individuals, and both of those were subsequently treated with complete relief of their symptoms. These positive results reveal a minimally invasive treatment that may be an alternative to traditional surgery.”
SIR, a national organization of nearly 4,700 doctors, scientists and allied health professionals dedicated to improving health care through minimally invasive treatments, annually sponsors Legs For Life, a nationwide community health and public information and PAD screening program. Legs For Life began a decade ago because interventional radiologists — vascular experts who treat PAD — recognized that the disease is a major public health problem with a growing incidence.
For more information: www.SIRweb.org
1. "Prevalence of Abnormal Ankle Brachial Index Among Individuals With Low or Intermediate Framingham Risk Scores," Rajoo Dhangana, M.D., Bridgeport Hospital, Bridgeport, Conn.; Timothy P. Murphy, M.D., FSIR, Sun-Ho Ahn, M.D., and Abdul M. Zafar, M.D., all Vascular Disease Research Center, Rhode Island Hospital and department of diagnostic imaging, Alpert Medical School at Brown University, Providence, R.I.; Joseph R. Coll, Ph.D., department of biostatistics and informatics, University of Colorado, Denver; Fathima F. Qadeer, M.D., department of psychiatry, Duke University, Durham, N.C.; William R. Hiatt, M.D., department of medicine, division of cardiology, University of Colorado School of Medicine and CPC Clinical Research, Aurora, Colo.
2. "Bifurcated Endograft in Aorto-iliac Type C and D Lesions: Long-term Results," Tobias Zander, M.D.; Oscar Blasco, M.D.; Martin Rabellino, M.D.; Sebastian Baldi, M.D.; Elisabeth Sanabria, M.D.; Manuel Maynar, Ph.D., M.D., FSIR, all department of endovascular therapy; Rafael Llorens, M.D. and Ignacio Zerolo, M.D., department of cardiac surgery; Luis Garcia, M.D., department of interventional cardiology, all Hospital Hospiten Rambla, Tenerife, Spain.


 September 12, 2025
September 12, 2025