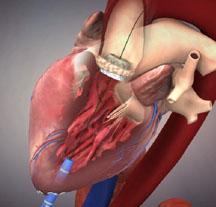
If approved by the U.S. Food and Drug Administration (FDA) later this summer, transcatheter valve therapy (TVT) – an innovative procedure that uses minimally invasive catheter-based technology to repair heart valve disease much like stents with coronary arteries – will bring a new therapeutic option to older patients with aortic stenosis who either could not be treated before or are too high-risk for conventional surgical therapy. Because of the anticipation and issues surrounding its potential release, its complexity and the multitude of stakeholders with a vested interest, the American College of Cardiology Foundation (ACCF) and The Society of Thoracic Surgeons (STS) today released a joint position statement to identify and provide timely guidance on key clinical issues that will arise with the potential roll out of this new technology, as well as recommendations for how to optimize patient safety and outcomes.
“This technology represents a major advance in science that will greatly benefit certain patients, but care must be taken to assure its appropriate use,” said Michael J. Mack, M.D., FACC, president of STS. “There need to be careful parameters for the clinical introduction of this therapy, including what we are calling a ‘rational dispersion’ of the technology to centers with a specialization in valvular disease and a multidisciplinary team of cardiologists and surgeons working together. Patients will need to be screened and followed very carefully. We hope this document provides the framework to build transcatheter valve programs.”
The ACCF/STS document, which was peer-reviewed by more than two dozen physicians representing a mix of cardiac surgeons and primary and interventional cardiologists, sets forth specific recommendations for the successful introduction of this therapy, including:
· Specialized heart centers that have significant experience in treating heart valve disorders. Not every hospital with a catheterization lab or operating room should be performing this procedure. According to the authors, TVT should be viewed as a program rather than a procedure -- analogous to heart transplantation programs for which a myriad of specialists, proper facilities and infrastructure are needed for optimal results.
· Multidisciplinary heart teams that include primary cardiologists, cardiac surgeons, interventional cardiologists, echocardiographers and imaging specialists and heart failure specialists. Because the results of the PARTNER trial were obtained in high volume centers with extensive and cooperative surgical and cardiology experience in treating patients with heart valve disease, this model needs to be replicated as it moves out to other centers.
· Proper procedures and facilities. TVT needs to be performed in what are called hybrid operating rooms or modified cath labs that are able to maintain surgical sterility, are large enough to accommodate all of the equipment needed and have the same superior imaging capability found in conventional cath labs.
· Development of national registries to evaluate post-market practice patterns and treatment outcomes. ACC and STS are working together with the trial sponsor and regulators to form a new national registry to track patients long-term after they receive this therapy; both societies already have large clinical databases that collect and analyze outcomes of surgical and catheter-based procedures to form the foundation for this registry.
· Review of current and future scientific studies. To date, initial experience is based on one randomized clinical trial in patients with aortic stenosis (PARTNER) as well as multiple registry experiences, so there will need to be ongoing evaluation of emerging study results and comparative effectiveness studies to determine the appropriate role for this new therapy as it evolves.
· Standardized protocols for training physicians on how to appropriately use this therapy.
Moreover, there needs to be measured clinical uptake of this therapy. As promising as it appears, authors caution that it is not for everyone.
“While this therapy will be an option for elderly patients with heart valve problems who either had been considered inoperable or had been deemed too high risk for surgery, some will be too old, too debilitated or sick even for the transcatheter aortic valve replacement procedure,” Mack said.
Subsequent scientific studies and trials are also needed to understand if and how younger patients or lower-risk elderly patients might benefit. The professional societies also feel a strong need to move beyond potential competing influences between specialties, according to the authors, which is why these two groups are working together to shape the dialogue around how to best integrate this new technology.
“We need to provide optimal care above all else, and patients like less invasive options if there are good outcomes,” said David R. Holmes, Jr, M.D., FACC, president of ACC. “The focus has to be on the patient and not on a specialty or the specialist doing the procedure. It is crucial that ACC and STS work together from the start – even before this technology is commercially available – to avoid some of the tugs of war that have ensued in the past. Both specialties are integrally involved with different aspects of these patients and they bring different, but complementary skill sets to the table.”
An overarching goal of this effort is also to help align the interests of various expert physicians (e.g., cardiologists, cardiac surgeons, proceduralists, heart valve, heart failure and imaging specialists), regulators, payers, and professional societies to deliver the best possible patient-centered care and judiciously introduce this innovative technology into select centers.
“Both ACC and STS are committed to providing guidance to various stakeholders as this new technology unfolds,” Holmes said. “This position statement presents a 30,000 foot view of the issues that need to be addressed – for example, how this therapy will be rolled out, which centers will be selected, who will train operators, and so on. It also helps set the stage for subsequent documents that are being written in collaboration with other professional societies.”
Two of the forthcoming documents include:
· Appropriate training qualifications and credentialing for physicians and centers to perform this procedure (being developed collaboratively by ACCF, STS, the American Association for Thoracic Surgery, and the Society for Cardiovascular Angiography and Interventions).
· An expert consensus document by the same professional societies plus others to assess the current state of knowledge about transcatheter valve therapy and how this technology should be used.
The full statement will be published in The Journal of the American College of Cardiology and The Annals of Thoracic Surgery.
For more information: www.cardiosource.org/ACC


 December 24, 2025
December 24, 2025 









