September 7, 2010 - With increasing rates of patients with atrial fibrillation program suffering from severe strokes, medical associations fear an epidemic. New developments in minimally invasive therapy of atrial fibrillation are booming and will be evident at MEDICA 2010, World Forum for Medicine - International Trade Fair and Congress, to be held from Nov. 17 – 20, 2010, in Düsseldorf, Germany.
Fifteen to 20 percent of all strokes are caused by atrial fibrillation, and these strokes are usually very severe. Atrial fibrillation is the most common cardiac arrhythmia. In Europe, more than 6 million primarily older people are affected, about 1 million in Germany alone. Epidemiologists expect that the year 2050 will see approximately 2.5 times more patients with atrial fibrillation.
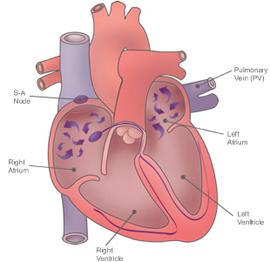
Catheter ablation is an established invasive procedure for cases of atrial fibrillation, in which a special catheter is inserted right to the heart through the veins in the groin. This procedure is usually applied if treatment with drugs has not had satisfactory results. With this minimally invasive procedure, the junction area of the pulmonary veins is electrically isolated in the heart (known as pulmonary vein isolation).
Whereas pulmonary vein isolation (PVI) is generally sufficient for cases of paroxysmal atrial fibrillation (PAF), chronic atrial fibrillation (CAF) requires a significantly more complex procedure with frequent repeated surgical interventions.
Today, the success rate of PVI is between 60 and 80 percent. As a large part of atrial fibrillation recidivation is asymptomatic after ablation, not all episodes of atrial fibrillation can be recorded through conventional observation. However, experience shows that the majority of patients who are highly symptomatic prior to ablation will, during the course, again experience at least some of the episodes.
Good Results With the Cryo Technique
An alternative procedure to PVI with high-frequency current is balloon catheter ablation. The application of high-intensity focused ultrasound (HIFU), cryothermal (cryo) or laser energy can generate circular lesions. The success rate is similar to that of high-frequency energy. However, HIFU ablation had to be withdrawn from the market because of serious complications (esophageal fistulas).
Good results can be achieved with the cryo technique: With PAF, the freedom from recidivation over a period of 12 months is 74 percent. The main problem with the application of balloon catheters is the comparatively high incidence, five to 10 percent, of paralysis of the right phrenic nerve. A disadvantage of the balloon catheter is its exclusive use for PAF. In contrast, the advantage of cryoenergy is that no atrio-esophageal fistulas have been observed to date. Up to now, only initial reports are available on the laser procedure, whose success rate after 12 months is 60 percent.
Robot-Aided Systems Offer Advantages
The main concern in catheter therapy is, of course, maximum precision in conjunction with minimum treatment time and low radiation exposure. Robots offer several advantages in this regard. As one of the first hospitals in Germany to do so, the University Hospital of Heidelberg began using a robot-aided system about one year ago. With this system, the physician sits at a console and, by means of a 3-D computer mouse, controls the catheter inserted into the heart and obliterates the cardiac tissue.
With this robotic system, Sensei from Hansen Medical, it is possible to reach regions of the heart that are difficult to access. Tissue contact is continuously monitored via a special sensor. With this 3-D, computer-aided procedure for localization diagnostics, the intervention is not dependent on X-rays and significantly reduces radiation exposure.
In recent months, cardiologists at the Bergmannsheil University Hospital in Bochum, Germany, have been using a special new catheter. The reason is that the previous procedure was very complex; with a catheter tip of mere millimeters, the scars had to be created point by point. The entire procedure could last up to eight hours. The Ablation Frontier catheter system from Medtronic had the solution.
“On the head of this new catheter is an annular terminal with a number of platinum electrodes through which electric current flows,” explains Dr. Thomas Lawo, senior physician at the Hospital for Cardiology and Angiology. “This allows us, comparable with a stamp, to isolate a circular-shaped piece of tissue in a single procedure. The new catheter reduces the duration of the procedure to less than two hours.”
As less energy is applied with this treatment, the procedure is more gentle and less stressful for the patient. “Almost 80 percent of patients are completely or almost completely healed with this procedure,” said Lawo's colleague Dr. Leif Ilja Bösche.
Since the beginning of this year, the cardiologists of the Heart and Diabetes Centre in Bad Oeynhausen, Germany, have been using a gold-plated catheter. However, what is special about this high-end catheter system is not just the gold plating, but also that the catheter tip is controlled by means of a magnet. Up until now, control has mostly been manual. Users said ablation guided by magnets offers many advantages.
The magnets allow continuous contact between the catheter and the tissue to be obliterated. This achieves not only better results in the case of complex treatments, but there are also fewer complications from applying too much pressure when pressing the catheter onto the walls of the heart. The gold catheter ensures a high degree of precision energy transmission and significantly reduces the risk of clotting and consequently stroke.
More Options in Pharma Therapy
Pharmacotherapy for atrial fibrillation is currently also making advances. Cardiologists now have considerably more options when it comes to effective drugs, albeit available on prescription only. For instance, in Germany the anti-arrhythmic drug Dronedaron (Sanofi-Aventis) has been on the market since January. In one certification study, compared to placebos in conjunction with standard therapy it reduced the risk of having to be admitted to a hospital for cardiovascular reasons or the risk of death by any cause by 24 percent (incidence: 31.9 versus 39.4 percent). According to a further analysis, Dronedaron also reduces the incidence of stroke by 34 percent (1.8 versus 1.2 percent).
It was called a paradigm shift in therapy when study data regarding the anticoagulant Dabigatran (Boehringer Ingelheim) was presented in 2009. More than 18,000 patients with atrial fibrillation took part in that RE-LY-study (RE-LY = randomized evaluation of long-term anticoagulant therapy). The results showed that both dosages (110 and 150 mg twice a day) of the preparation were better than the “gold standard” of warfarin in preventing stroke and systemic embolism, without an increase in the incidence of hemorrhagic stroke.
And just months ago the study data on the new anti-arrhythmic drug Vernakalant were presented. In a phase III study, the new active agent (from MSD and Cardiome Pharma) had significantly better results than the classic Amiodaron, even when it comes to quality of life.
At MEDICA 2010, the status of modern therapy with respect to atrial fibrillation will also be a topic at the congress event, “Atrial Fibrillation Update,” held from 10 a.m. to 1 p.m. Thursday, Nov. 18, 2010, in the Congress Center South.
For more information: www.medica-tradefair.com


 January 28, 2026
January 28, 2026