July 2, 2009 – Researchers from Dartmouth-Hitchock Medical Center (DHMC) in Lebanon, N.H., have published a new study in the July issue of the Journal of Vascular Surgery (published by the Society for Vascular Surgery) about the trends in lower extremity endovascular interventions (angioplasty and atherectomy), lower extremity bypass surgery and major above and below the knee amputations in Medicare beneficiaries (Part B claims). The study was done between 1996 and 2006.
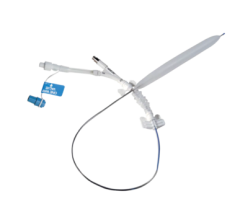
Lower extremity peripheral arterial disease (PAD) affects more than 8 million Americans, with significant risks of limb loss, disability and death. Treatment of lower extremity PAD focuses on restoring normal blood supply to the affected limb. Traditional treatment, such as surgical bypass, is effective but invasive. In recent years, many patients have been treated with newer endovascular interventions, using catheter-based devices to reopen peripheral arteries in a less-invasive fashion. According to past research, it is unclear if these newer treatments are as effective as conventional surgical bypass in preventing amputation.
Philip P. Goodney, M.D., from the DHMC section of vascular surgery, noted that endovascular interventions were now performed much more commonly than bypass surgery in the treatment of lower extremity PAD. Across the United States, more than three endovascular interventions replaced every single decline in lower extremity bypass surgery over the last 10 years.
"During the study period, per 100,000 patients, bypass surgery rates decreased from 219 to 126 procedures (43 percent); endovascular interventions increased from 138 to 455 procedures (230 percent), and the rate of lower extremity amputation rates fell by 28 percent from 263 to 188," said Dr. Goodney.
Increased numbers in endovascular interventions per 100,000 patients was due to growth in peripheral angioplasty (from 135 to 337 procedures) and percutaneous atherectomy (from three to 118 procedures), according to researchers, who added that percutaneous atherectomy is a particularly new, expensive and relatively untested treatment – however its rate has increased by more than 4,100 percent.
"We suspect new procedures may have translated into better outcomes, given the significant decline in amputation rates. However, other aspects of health care provided to patients at risk for amputation have changed along with the rates of surgical and endovascular procedures," added Dr. Goodney. "Medicare patients are much more likely to receive medical and podiatric care, such as cholesterol monitoring, diabetic foot examinations and blood glucose monitoring aimed at preventing amputation now than they were 10 years ago. Our future work aims to determine if amputation rates are falling because of better medical care, changes in revascularization strategies or a combination of the two."
Dr. Goodney said that larger and broader clinical trials should occur to compare bypass and endovascular interventions in patients with claudication and critical limb ischemia. These trials would further evaluate what medical steps can be taken and resources should be used to obtain the best functional outcomes in patients with PAD, and to prevent death and disability from lower extremity amputation.
For more information: www.jvascsurg.org, www.VascularWeb.org

 June 13, 2024
June 13, 2024 









