December 17, 2007 - Patients treated with drug-eluting stents must take a combination of aspirin and the clot-reducing drug clopidogrel for at least one year, and possibly longer, after stent implantation, according to a guideline update published online today in the journals of the Society for Cardiovascular Angiography and Interventions (SCAI), American College of cardiology (ACC) and American Heart Association (AHA).
"For most patients suffering a heart attack, angioplasty and implantation of a stent is a life-saving procedure," said SCAI President Bonnie Weiner, M.D. "However, both patients and the medical community need to understand how essential dual anticoagulant therapy is after receiving a drug-eluting stent. That's the purpose of this update -- to stress this and other evidence published relatively recently."
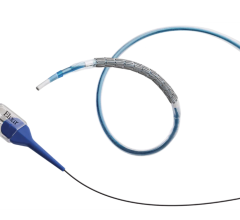
The update specifically addresses findings from studies published through late 2006. One of the concerns that arose during this period was about a slightly higher risk of blood clots forming inside drug-eluting stents. These clots are a rare but serious complication of drug-eluting stents and must be prevented with a strict regimen of aspirin plus the clot-reducing drug clopidogrel for at least one year after the artery is opened with a stent. "By emitting tiny amounts of medication, drug-eluting stents reduce the regrowth of scar tissue and other build-up that could renarrow the artery, creating a need for a repeat angioplasty," explained Dr. Weiner. "While we don’t want to understate the precautions that should be taken to prevent clots, we also want to factor in the benefits of these newer devices.
"If there are doubts about whether the patient can stay on the dual-antiplatelet therapy for at least one year, then a bare metal stent is probably the better choice," stresses Dr. Weiner. "We want to encourage physicians to think about the patient's history with compliance to drug therapy as well as other potential obstacles, such as planned surgeries, that might lead them to not take their aspirin and clopidogrel. In those cases, the update calls for a bare metal stent or balloon angioplasty with provisional stent implantation."
The guideline update also considers OAT (Open Artery Trial) and the earlier ICTUS (Invasive versus Conservative Treatment in Unstable coronary Syndromes) study, two randomized clinical trials that looked at whether to open totally blocked arteries in patients who had suffered a heart attack between three and 28 days earlier. "OAT looked at patients with a completely blocked artery who had suffered a heart attack between 72 hours and 28 days earlier, but had neither serious chest pain nor evidence of ischemia," said Dr. Weiner. "Considering the findings of ICTUS, the writing committee suggests that in patients with unstable angina or the milder form of heart attack known as non-ST-segment elevation myocardial infarction (NSTEMI), risk stratification is critical to determining the optimal approach to patient care and that coronary angiography and PCI improve outcomes in high-risk patients."
"The OAT findings might rule out a small subset of patients who might have otherwise been candidates for angioplasty," said Douglass Morrison, a writing committee member and an OAT investigator, "but it also points to a very important issue: time. The real emphasis needs to be on educating patients to call 9-1-1 if they are having heart attack symptoms so they can get to the emergency department in time to have PCI when it will do the most good."
The update also strengthens the earlier guideline’s recommendations about smoking cessation, exposure to second-hand smoke, medical management of high cholesterol and high blood pressure, coordinated care of diabetic patients and getting a flu shot. The update does not address in detail when PCI should be used for patients with chronic stable angina. The more recent studies addressing this issue are still being tested in ongoing studies and debated in the medical literature.
For more information: www.scai.org


 July 02, 2024
July 02, 2024