October 8, 2007 - Drug-eluting stents were found to be most effective in reducing the need for repeat angioplasty procedures or bypass surgery in angioplasty patients at the ‘highest risk for a renarrowing of the artery around the stent, without significantly increasing the rate of death or risk of heart attack, said a new study by Ontario’s Institute for Clinical Evaluative Sciences (ICES) and McMaster University’s Program for Assessment of Technologies in Health.
Lead Author, ICES Sr. Scientist, Jack Tu, M.D., said, “Our results also suggest physicians should be selective in using drug-eluting stents, offering them to angioplasty patients who are at the highest risk for repeat cardiac procedures.”
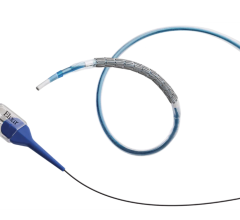
Reporting in the October 4th issue of the New England Journal of Medicine, the large Canadian study conducted at ICES, in collaboration with cardiologists and researchers from Sunnybrook Health Sciences Centre and the University of Toronto, looked at over 3,700 unique matched pairs of Ontario patients who received drug-eluting stents (DES) or more conventional bare metal stents (BMS) during angioplasty. Using data from the Ontario Cardiac Care Network's (CCN) population-based angioplasty registry, and accounting for differences in patient characteristics, investigators analyzed the outcomes of patients having angioplasty in Ontario between December 2003 and March 2005 for the 'real-world' effectiveness of DES. The results:
- DES reduced the need for a second procedure to unblock or bypass a clogged artery by 30 percent relative to BMS, from 10.7 percent to 7.4 percent.
- After three years of follow up, mortality was reduced for DES patients (5.5 percent) relative to BMS (7.8 percent).
- After two years of follow up, rate of heart attack for DES patients was marginally but not significantly higher at 5.7 percent vs. 5.2 percent in BMS patients.
- The reduction in the need for repeat procedures (i.e. target vessel revascularization (TVR rate)) was greatest in patients with two or three risk factors (e.g. diabetes, small vessels, or long lesions) for renarrowing of the artery, whereas lower and intermediate risk patients did not have significant reductions in TVR rates.
Author affiliations: ICES (J.V.T., M.C., D.T.K., P.C.A., Y.H.) and Sunnybrook Health Sciences Centre, University of Toronto (J.V.T., D.T.K., E.A.C.) - both in Toronto; McMaster University, St. Joseph's Healthcare, Hamilton, ON (J.B., R.H., J.-E.T., G.B., R.G.); and Trillium Health Centre, Mississauga, ON, (C.L.) - all in Canada.
Source: Institute for Clinical Evaluative Sciences
For more information: www.ices.on.ca


 July 02, 2024
July 02, 2024