May 31, 2007 - The American Heart Association is launching a community-based program to reduce the toll of the deadliest kind of heart attack: an ST-elevation myocardial infarction (STEMI).
The total blockage of a coronary artery is fatal unless treated quickly — within 30 minutes for clot-dissolving drug treatment, and within 90 minutes for angioplasty.
But, the “HealthDay Reporter” writes today, fewer than half of all STEMI patients get the right treatment at the right time, according to Dr. Alice Jacobs, professor of medicine at Boston University and past president of the heart association, who described what the association is calling "Mission Lifeline."
The program's emphasis will be to improve on the current treatment statistics, Jacobs said. "Thirty percent of STEMI patients do not get clot-busting drugs," she said. "Twenty percent are not candidates for clot-busting drugs and, of these, 70 percent do not get angioplasty."
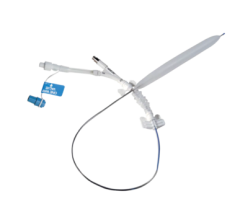
A major part of the effort will be devoted to establishing systems to transport STEMI patients to hospitals that are equipped to do angioplasty. The reason: "Angioplasty is better than clot-busting treatment, even when transportation is needed," Jacobs said. Only 25 percent of U.S. hospitals have the catheterization facilities that allow them to do emergency angioplasties, she said.
But another major component of the program will be devoted to teaching people in general to call 911 for emergency help when they experience symptoms of a heart attack. About half of all heart-attack patients now drive themselves to a hospital or are driven.
That adds up to a shocking loss of time when they could be getting emergency therapy, and the hospital could be preparing for their arrival, said Dr. Tim Henry, director of research at the Minneapolis Heart Institute.
The institute has a program that the heart association hopes will be a model for rural areas. It ties together more than 100 hospitals, most of which cannot do angioplasty. There had been doubts about whether patients could be transferred quickly enough for angioplasty to be done on time. But, Henry said, "We now have 31 hospitals trained up to 60 miles away, then out to 210 miles away. A 60-mile transfer can be done in 95 minutes, and a 200-mile transfer can be done in 120 minutes."
"The mortality of these patients is now 4 percent," Henry added, a figure that is impressive, because 15 percent of those transferred are over 80 years of age.
Comparable local programs in areas such as North Carolina and California also can serve as models, Jacobs said. Those programs were taken into consideration at a three-day conference in March where experts agreed on starting the nationwide effort. Details of the conference are published in the May 30 online edition of the heart association journal Circulation.
The program will start with individuals at risk of a heart attack, Henry and Jacobs said. It's important for those people to seek trained help as quickly as possible by calling 911, Jacobs said.
There are no estimates of how much the program will cost or where the money will come from, but there is the potential for saving money as well as lives, Henry said. Quick, appropriate treatment can translate into shorter hospital stays and reduced need for expensive medical technology such as implanted defibrillators, he said.
Only 3 percent of people treated in the Minneapolis program get defibrillators, Henry said.
For more information visit www.americanheart.org

 June 13, 2024
June 13, 2024 









