June 29, 2018 — Results from the MERCURY PE study showed that low-risk pulmonary embolism (PE) patients treated with Xarelto (rivaroxaban) and discharged early from the emergency department had significantly reduced time in the hospital and a median savings of $2,496 per patient. MERCURY PE results were published in Academic Emergency Medicine.
"Every year, U.S. healthcare systems spend more than $2 billion to manage patients with pulmonary emboli," said principal study investigator W. Frank Peacock, M.D., FACEP, FACC, associate chair and research director, emergency medicine, Baylor College of Medicine, Houston. "By avoiding hospitalizations that are not clinically necessary and transitioning patients with low-risk PE to outpatient treatment with Xarelto, we've seen significant cost savings, which could help alleviate the burden on health care systems."
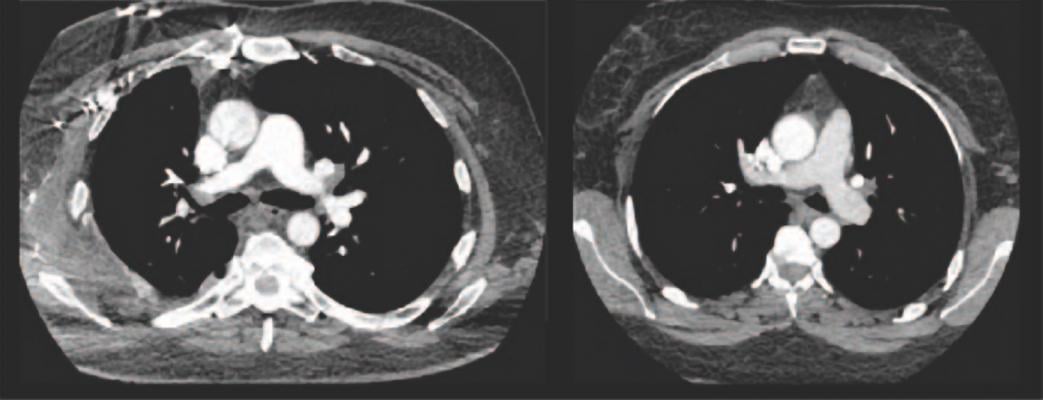
Venous thromboembolism (VTE) includes deep vein thrombosis (DVT), a blood clot in a deep vein, and PE, a potentially life-threatening condition that occurs when a blood clot travels to the lung. Of the approximately 900,000 Americans who experience a VTE each yeari, more than 250,000 are diagnosed with PE in the emergency departmentii. Hospitals across the United States have varying protocols for managing PE, but standard of care typically requires people to be admitted for treatment, which drives up costs and substantially increases hospital-acquired conditions and infectionsiii,iv. While people with more severe PE have higher mortality rates, the 30-day mortality rate of low-risk PE is less than one percentv.
MERCURY PE met its primary efficacy endpoint, with Xarelto leading to significantly reduced time in the hospital due to VTE or bleeding within 30 days after randomization compared with the standard of care (mean duration of 4.8 vs. 33.6 hours, respectively; 95% CI; p<0.0001). The mean difference of length of stay between the two groups was 28.8 hours. Of note, there was no recurrence of VTE or VTE-related death, or any significant differences in the bleeding-related hospitalizations or physician visits within 90 days from randomization in either group. This outcome should be interpreted with caution, the researchers said, as the study was significantly underpowered to detect any such differences.
In MERCURY PE, patients with low-risk PE were randomly assigned in a 1:1 ratio to open label Xarelto or standard of care within 12 hours of diagnosis. Patients randomized to Xarelto were discharged from the emergency department within 24 hours and were instructed to take Xarelto 15 mg twice daily for 21 days, then 20 mg once daily until the study was completed. Patients randomized to standard of care were treated per local hospital protocol, which could include hospitalization and any U.S. Food and Drug Administration (FDA)-approved anticoagulant strategy, including Xarelto.
Researchers also made the following observations about Xarelto in this setting:
- The mean length of initial and subsequent hospitalizations for any reason was shorter for patients who were discharged early on Xarelto within 90 days from randomization compared to those receiving standard of care (p=0.024; 19.2 hours vs. 43.2 hours, respectively);
- There was no major bleeding in either group within 90 days from randomization, although two patients reported clinically relevant non-major bleeding, one in each group. There were no deaths due to bleeding in the study; and
- Overall, early discharge on Xarelto was markedly less expensive than standard of care. The cost associated with the emergency room visit and any subsequent hospitalization at the time of PE diagnosis and the total costs were $2,638 (p<0.001) and $2,496 (p<0.001) less with Xarelto.
MERCURY PE builds on prior research, including a June 2015 study published in Academic Emergency Medicine. That study showed that 106 patients with low-risk PE or DVT, when prescribed Xarelto and immediately discharged, had no recurrent events while on therapy. Additionally, no major or clinically relevant bleeding events were observed. A companion study found patients with low-risk PE or DVT who were prescribed Xarelto had significantly lower medical costs than those admitted and given standard treatment.
The clinical and economic benefits demonstrated in the MERCURY-PE trial have been confirmed in more than 3,100 U.S. patients in a real-world study. That study showed that Xarelto resulted in a significant one-day reduction in hospital length of stay and significantly lower total healthcare costs (approximately $2,000).
Patient satisfaction, both with out-patient and in-patient care, was also analyzed using Likert scales and the Anti-Clot Treatment Score (ACTS). On the Likert scales, most patients in both groups indicated they were "very satisfied" with their care, but numerically more patients taking Xarelto preferred to receive outpatient care (50 percent) compared to slightly less than half of patients receiving in-patient standard of care (47.5 percent). The ACTS measured the patient's perspective on the burden of treatment, with more patients taking Xarelto reporting it was "not at all" burdensome compared to those receiving standard of care (64.4 percent vs. 54.4 percent).
For more information: www.onlinelibrary.wiley.com
References


 August 28, 2023
August 28, 2023 









