September 25, 2018 — Orchestra BioMed Inc. announced the three-year clinical results from its Sirolimus Angioplasty Balloon for In-Stent Restenosis (SABRE) Trial at the Transcatheter Cardiovascular Therapeutics (TCT) 2018, Sept. 21-25 in San Diego. Results demonstrated excellent efficacy and safety performance of the Virtue Sirolimus-Eluting Balloon (SEB) in a very challenging patient population with predominantly long, diffuse restenosis lesions within stents that had been implanted an average of nearly four years prior to the study enrollment.
The primary safety and efficacy per protocol endpoint results of the study were as follows:
- Zero percent major adverse cardiac events (MACE) in hospital and at 30-day follow-up;
- 0.12 mm late lumen loss (LLL) at six-month angiographic assessment;
- Five-point-six (5.6) percent target lesion failure (TLF) at three years; and
- No target lesion revascularization (TLR) events following six-month angiographic assessment.
Juan Granada, M.D., associate professor of medicine at the Columbia University College of Physicians and Surgeons and president and CEO of Cardiovascular Research Foundation, presented the outcomes of the SABRE trial.
“We still do not have a perfect solution for the treatment of late stent failures and the three-year results of the SABRE trial are very encouraging in the search to find a ‘leave nothing behind solution’ with a favorable safety profile and biological efficacy comparable to proven drug-eluting stents,” said Granada.
“The clear biological efficacy demonstrated by this study, despite complex and challenging cases, was consistent with the effective therapeutic delivery of sirolimus during angioplasty. The results with Virtue SEB compare favorably to proven drug-eluting stents (DES) and paclitaxel-coated balloons (PCB) and outperform PCBs in some key safety metrics observed in other coronary in-stent restenosis trials,” commented Stefan Verheye M.D., senior interventional cardiologist at Antwerp Cardiovascular Center, ZNA Middelheim, Antwerp, Belgium and principal investigator in the SABRE study.
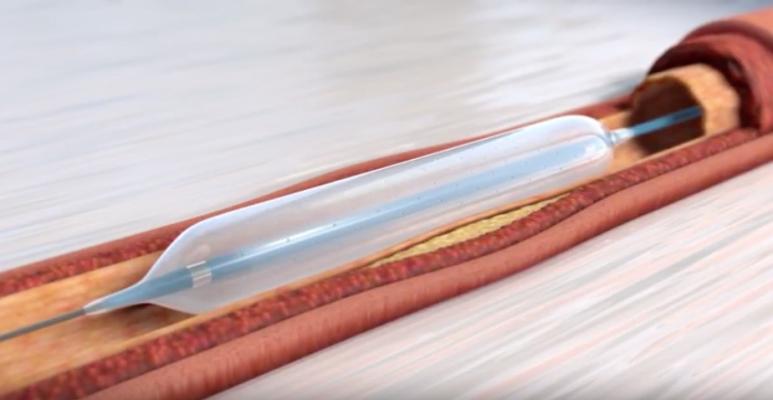
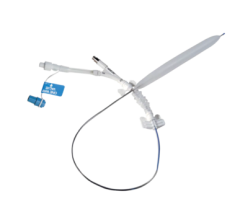
The SABRE trial was a prospective, 50-patient multi-center study conducted in European centers. Twelve-month follow-up data from the SABRE study was published in JACC: Cardiovascular Interventions, October 2017. Clinicians in the study had 100 percent procedural success rate (per patient) with Virtue SEB, indicating the ease of use of the system. By enabling the simultaneous delivery of a full therapeutic dose of sirolimus during angioplasty, the device aims to address long-term issues associated with late adverse events following treatment of coronary arteries with stents, which are permanent implants.
Although the original introduction of bare metal stents (BMS) significantly improved short-term outcomes observed with plain balloon angioplasty, extensive data shows late adverse events occur at an annual rate of approximately 2.1 percent following the year after implantation. Drug-eluting stents (DES), which currently exclusively utilize sirolimus or chemical analogs, were introduced to further advance the treatment of coronary restenosis. While the presence of a drug immediately following the implantation dramatically improved the TLF rates in the first year after implantation over BMS, longer term TLF rates are higher (2-4 percent/year) even with second-generation DES. It is believed that the long-term events are driven by the permanent presence of a metal stent in the artery. Bioabsorbable stents, led by the Absorb GT1 Bioabsorbable Vascular Scaffold (Abbott), were designed to overcome the permanent implant issue by dissolving over 24-36 months following implantation and showed promising short-term outcomes. However, at three years, Absorb GT1 Bioabsorbable Vascular Scaffold was associated with statistically significant higher rates of late stent-related thrombosis than DES, and Abbott has halted commercial sales of the product.
Clinical interest to eliminate the need for a permanent stent is perhaps strongest in cases of coronary in-stent restenosis (ISR), where the off-label placement of an additional stent on top of the original stent has been shown to drive an increase in long-term TLF. While angioplasty balloons coated with the cytotoxic agent paclitaxel have been approved in the U.S. for the treatment of the superficial femoral artery and have shown promise outside the U.S. for the treatment of coronary ISR, sirolimus is the gold-standard pharmaceutical agent used in conjunction with coronary stenting to prevent restenosis (reclogging) of an artery following percutaneous coronary intervention (PCI), as extensive clinical data demonstrated clinical superiority to paclitaxel. Further, drug-coated balloons present potential concerns associated with the safety risk of creating large size particulate from the coating that block smaller vessels distal to treated lesions.
For more information: www.orchestrabiomed.com

 June 13, 2024
June 13, 2024 









