September 8, 2008 - A new procedure being pioneered by Dr. Nassir Marrouche, director of the atrial fibrillation (AF) program at the University of Utah School of Medicine, Salt Lake City, could represent a breakthrough in the treatment of AF using MRI-guided imaging.
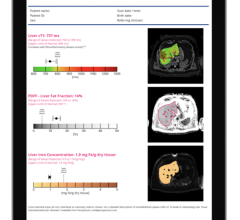
Dr. Marrouche and his team are among the first researchers in the country to use magnetic resonance imaging (MRI) to refine image-based ablation procedures. They are able to locate precisely where errant electrical signals originate and assess how much damage the heart has sustained. Since the MRI lab is next to the catheter lab, they can check to see if signals are still present after a procedure, and go back to the cath lab to burn more tissue if necessary. Dr. Marrouche has used MRI in more than 230 cardiac ablation procedures, and about 90 percent of these patients are arrhythmia free and off heart medications within three months.
For Lisa Wheeldon and Charles Hawker, this scientific advancement has meant freedom from debilitating drugs and the promise of a better quality of life.
“Dr. Marrouche is my star,” said Wheeldon, 80, of West Jordan, UT, who had had several previous surgeries for her AF. “A few years ago my doctor took me off of a heart medication, which was poisoning me. Dr. Marrouche did my surgery last July and since then my heart rhythm has been normal. He told me, ‘Lisa, go out and live your life.’”
Atrial fibrillation, often known as afib, is a misfiring of the electrical signals of the heart that cause rapid and/or irregular heart beats. A common treatment for AF patients is radiofrequency ablation, which involves the use of catheters to burn away damaged heart tissue. The risks in such procedures are that not enough tissue will be burned, requiring the patient to undergo the procedure again, or that too much tissue will be burned, resulting in a rare but fatal complication. Even though physicians have been performing these procedures for years, their overall success rate has only been about 50 percent.
“I work with technology every day, and this is space age stuff,” said Hawker, 68, a biochemist and the scientific director at ARUP Laboratories at the University of Utah. “With the sensors in your heart, the doctors can see the electrical impulses flash, and they zap them, just like in Star Wars.”
Hawker was diagnosed with AF in April 2007 during an annual physical and was prescribed two drugs, which exacerbated his asthma and had other severe side effects. Last December he underwent an ablation surgery performed by Dr. Marrouche and now says, “I’m off those lousy medications, which I hated, and feel great. I had the procedure on a Wednesday and could have gone back to work in a Friday if I had wanted to.”
The non-profit organization, StopAfib.org, proclaimed September 2008 as Atrial Fibrillation Month to raise awareness of a disorder.
Last October, the University of Utah AF program became the first in the world to be able to ablate using a catheter custom-made to be compatible with MRI. By the end of the year, Dr. Marrouche plans to perform his first cardiac ablation procedure with simultaneous MRI imaging.
AF is a heart rhythm disorder that affects more than 3.5 million Americans and causes more than 66,000 deaths a year.
For more information: www.westernatrialfibrillation.com, www.StopAfib.org


 February 12, 2026
February 12, 2026