May 6, 2009 - University of Utah Health Care this week celebrated the opening of the first integrated electrophysiology (EP) MRI laboratory in North America.
Located on the fourth floor of University Hospital, the lab will accelerate the work of university physicians and researchers in diagnosing and treating atrial fibrillation (AF), a heart rhythm disorder affecting more than 3.5 million Americans and causing more than 66,000 deaths each year. University Health Care administrators, physicians, and staff joined with AF patients, donors, and Siemens executives for a ribbon-cutting ceremony and tours of the lab on Monday.
The new lab is a multi-disciplinary partnership between University Hospital, the university’s division of cardiology, department of radiology, Scientific Computing and Imaging Institute, and the Utah Center for Advanced Imaging Research (UCAIR). It features an 18,000-pound MAGNETOM 3T Verio from Siemens, which offers some of the most advanced magnetic resonance imaging (MRI) services clinically available, the hospital said. Officials said MRI’s 3D imaging provides greater resolution of the heart tissue than the 2D images typically used, giving physicians a more precise and powerful tool for diagnosis and treatment.
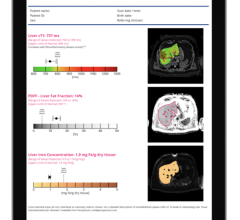
Nassir Marrouche, M.D., electrophysiologist and director of the university’s atrial fibrillation program, and his colleagues have conducted the most extensive studies to date on the use of novel MRI techniques for treating AF, an irregular heartbeat that interferes with the electrical signals of the heart. Left untreated, AF can lead to stroke or heart attack. A common and effective AF treatment method is radiofrequency ablation, which targets damaged heart cells and destroys them.
“We are refining image-based heart ablation procedures using MRI, which our research shows has the potential to improve the accuracy of the ablation, prevent complications, and decrease the number of repeat procedures,” said Marrouche. “These advances mean better outcomes for our patients.”
Initially, physicians will use the MRI equipment to diagnose appropriate candidates for cardiac ablation. They eventually will use the magnet for performing cardiac ablations using real-time MRI imaging.
The new lab also includes an Artis zeego angiography system, which is used for interventional imaging of the blood vessels and arteries and includes industrial robotic technology. According to E. A. “Steve” Stevens, M.D., professor and chair of the department of radiology, “We are combining two unique imaging technologies to increase the safety of ablative therapy and improve treatment outcomes. Our research shows that this technology integration will enable us to determine which patients with atrial fibrillation would be more likely to respond to ablative therapy and those for whom conservative therapy would be a better alternative.”
For more information: healthcare.utah.edu, medicine.utah.edu/internalmedicine/cardiology


 January 21, 2026
January 21, 2026