Image courtesy of Vital Images
February 9, 2015 — Ensuring that patients with peripheral arterial disease (PAD) get tested and treated with minimally invasive endovascular therapy saves legs and lives suggests a study in which amputation rates fell by nearly 80 percent after such a system was implemented. The research was presented at the 27th annual International Symposium on Endovascular Therapy (ISET).
About 150,000 Americans undergo leg or foot amputations every year mostly due to poor circulation caused by PAD. Eight to 12 million Americans – one in 20 who are 50 or older – have PAD, in which plaque builds up in blood vessels in the legs, decreasing blood flow. Because amputation has such a negative impact on quality of life, half of people who have the procedure die within 18 months.
“Most PAD patients don’t undergo testing to analyze blood flow first, they just have a leg or foot amputated,” said Julio Sanguily III, M.D., lead author of the study and vascular surgeon with Martin Health System, Stuart, Florida. “In recent years there has been a revolution in endovascular therapy and we’re able to treat calcified and smaller vessels, meaning we can significantly improve blood flow and save limbs that once weren’t considered salvageable. And that saves lives.”
He said the key is twofold: to educate physicians who treat elderly patients and those with diabetes or kidney failure – who are at highest risk for these problems – regarding the improved options and provide them the ability to refer patients to a limb salvage program that features a multidisciplinary team, including endovascular therapy specialists, podiatrists and other support staff.
The number of amputations at Martin Health System fell by 79 percent over five years after the center implemented a limb salvage program, ensuring patients with PAD have an angiogram – an X-ray of the blood vessels to assess blood flow. Significantly more people were evaluated as well, due to a program to increase awareness about PAD among patients and educate physicians regarding the options for their patients with PAD.
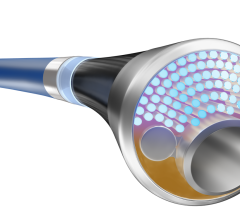
Whenever possible, the patients then received treatment to open up the blood flow in the legs, including angioplasty, other minimally invasive treatments such as atherectomy and hyperbaric oxygen therapy. Hardened or calcified plaque is the most challenging problem and atherectomy – a roto-rooter type device that removes plaque – has proved particularly helpful in treating patients with this problem, Sanguily said.
Each year significantly more Martin Health System patients were evaluated, yet the number who had amputations plummeted. In 2010, 24 of the 84 patients (29 percent) who were evaluated had amputations; in 2011, 146 were evaluated and 18 (12 percent) had amputations; in 2012, 228 were evaluated and 10 had amputations (4 percent); in 2013, 249 were evaluated and 6 had amputations (2 percent) and in 2014, 500 were evaluated and five had amputations (1 percent).
For more information: www.iset.org


 September 12, 2025
September 12, 2025