April 11, 2024 — Transcatheter aortic valve replacement (TAVR) was found to bring no increased risks and was associated with substantial decreased rates of death or stroke at one year in lowrisk patients, compared with surgical aortic valve replacement (SAVR), according to findings presented at the American College of Cardiology’s Annual Scientific Session.
TAVR and SAVR are procedures to replace a damaged aortic valve that is not functioning properly. U.S. guidelines recommend TAVR, a catheter-based approach in which the new valve is threaded to the heart through a blood vessel in the groin or chest, over open-heart SAVR for older patients and those with high cardiovascular risk. However, previous studies and different countries’ guidelines have varied when it comes to determining the optimal approach for younger and lower-risk patients.
“We can now provide strong data that in this low-risk patient population, you could very safely offer TAVR vs. SAVR,” said Moritz Seiffert, MD, professor of cardiology at BG University Hospital Bergmannsheil, Ruhr University Bochum in Bochum, Germany, and one of the study authors. “TAVR is less invasive; it’s usually performed under local anesthesia, lasting 30-60 minutes, and the convalescence is shorter than with open chest surgery. [These findings offer] a strong argument toward catheter-based treatment, at least for the one-year timeframe of this study, in these patients.”
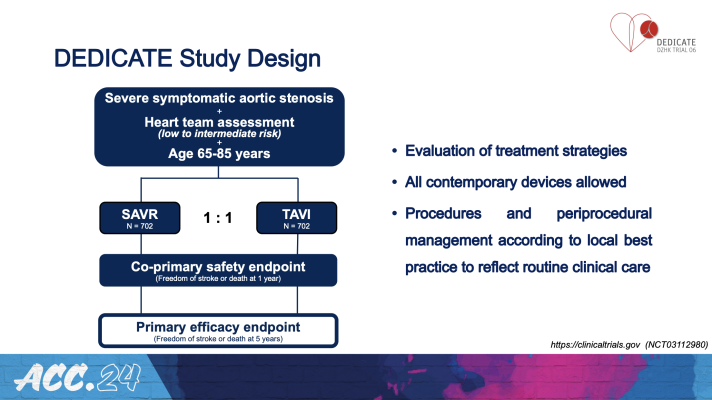
The DEDICATE-DZHK6 trial compared TAVR vs. SAVR in 1,414 patients who underwent valve replacement procedures at 38 centers in Germany.
All patients enrolled in the trial were eligible for either TAVR or SAVR and had similar characteristics in terms of the severity of aortic stenosis (narrowing of the valve which makes it harder for blood to flow efficiently) and a similar balance of risks and benefits expected with either type of procedure. Patients with bicuspid valves, previous heart surgery or additional coronary or valvular diseases requiring further treatment were excluded. The average age of participants was 74 years and 43% were women.
Researchers randomly assigned half of the participants to undergo TAVR and the other half to SAVR. Since the trial was intended to mirror real-world conditions, many decisions were left to the local heart teams at each study site, rather than strict predetermined study protocols. Local interdisciplinary heart teams determined which patients were eligible to participate in the study based on broad inclusion criteria. Operators selected which replacement valve to use and followed their own center’s standard practices for performing the procedures.
The co-primary safety endpoint was designed to assess whether TAVR was non-inferior to SAVR as indicated by an absolute increase of no more than 1% in the composite rate of death or stroke at one year. The trial met this endpoint, showing that people who underwent TAVR were 47% less likely than those undergoing SAVR to experience death or stroke at one year. Event rates for several secondary endpoints, including all-cause death or disabling stroke, were also significantly lower in patients undergoing TAVR compared with those undergoing SAVR at one year.
“Although we primarily tested for non-inferiority, the magnitude of the difference surprised us,” Seiffert said. “Valve prosthesis selection based on individual patients’ anatomical and medical considerations may have played a role. In addition, the COVID-19 pandemic might have amplified the surgical risk. In fact, the relative difference was comparable to previous studies, but the overall higher event rates and larger patient population may have led to these significant results.”
Researchers plan to further investigate some factors that set the trial apart from previous studies and may have contributed to the substantially reduced risk in the TAVR group, including the relatively high proportion of females in the study group. The data were consistent among the subgroups tested so far.
Overall, researchers said that the findings are likely generalizable to patient populations and health care environments across many developed countries.
“What it really adds to previous trials is that it mirrors clinical routine,” Seiffert said. “It’s completely industry independent, not focused on one particular device but comparing a catheter-based strategy to a surgical strategy overall. That makes it more applicable and aligned with the types of decisions physicians are making in their daily medical work.”
The researchers will continue to track outcomes for at least five years. Future analyses will include additional metrics for assessing clinical superiority as well as quality of life outcomes. In addition, researchers plan to examine whether certain subgroups appear to derive specific risks or benefits from one approach or the other.
The study was funded by German Center for Cardiovascular Research with financial support by the German Heart Foundation. This study was simultaneously published online in the New England Journal of Medicine at the time of presentation.
For more information: www.acc.org


 July 31, 2024
July 31, 2024 









