April 9, 2024 — Using a web application to qualify individuals for treatment with a nonprescription statin closely matched the results of clinician assessments in determining a person’s eligibility for taking statins to lower cholesterol, according to research presented at the American College of Cardiology’s Annual Scientific Session. Participants who were given access to a 5 mg dose of rosuvastatin using this technology-assisted approach experienced a 35.5% reduction in low-density lipoprotein (LDL) cholesterol, on average, six months after starting treatment.
The TACTiC trial is the first experiment with a prescription statin to show that consumers could selfselect correctly and take statins appropriately without requiring clinician qualification and a prescription.
Statins are a mainstay of heart disease prevention, yet experts estimate that less than half of patients who are eligible to receive the drugs are currently taking them. The new findings offer evidence that a web-based process allowing nonprescription access to statins could facilitate safe and effective use of the drugs, according to researchers.

Steven E. Nissen, MD
“We think this approach can make statins available to more people who are not currently taking these important drugs,” said Steven E. Nissen, MD, chief academic officer in the Heart, Vascular, and Thoracic Institute at Cleveland Clinic and the study’s lead author. “This therapeutic approach is designed to allow access to consumers who should be treated, while preventing access to those for whom statins are not indicated or unsafe.”
LDL or “bad” cholesterol contributes to the development of fatty deposits in the arteries, which raises the risk of heart attacks, strokes and other forms of heart disease. Statins help to remove cholesterol from the blood and reduce the amount of cholesterol the body produces, thereby lowering the risk of heart disease in people with high LDL cholesterol.
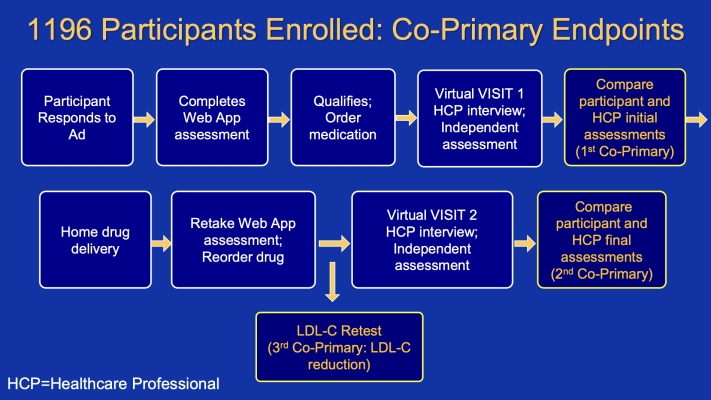
For the trial, researchers designed a system to make non-prescription statins available to the general population based on established eligibility criteria without requiring a doctor visit or prescription. First, people were invited to take a medical assessment using a web-based application designed as medical device software. The assessment required users to enter information about demographics, medication use, medical history, and cholesterol and blood pressure levels. If users did not know their cholesterol and blood pressure levels, they were given instructions on how to get this information, but no other assistance was provided.
Based on questionnaire responses, users were informed that they could use statins, could not use statins or should ask a doctor for further advice. Only those informed that they could use statins or should ask a doctor (and confirmed that they had done so) were eligible to set up an account and purchase medication. Participants could order up to a 90-day supply of 5 mg daily rosuvastatin, which they paid for and was shipped directly to their home. In total, 1,196 participants were enrolled; participants had a median age of 63 years and 39.6% were women.
After taking the self-assessment, participants were then interviewed by a clinician who determined whether they met the criteria for statin therapy. Clinicians were not aware of the responses or recommendations from the web-based assessment.
Next, participants entered the six-month treatment phase of the trial, which required them to reorder medicine and take an abbreviated web-app assessment prior to each reorder to ensure they continued to meet requirements for safe use. During this phase, participants were also instructed to have their LDL cholesterol re-tested at any point after starting treatment. At the end of the treatment phase, they were scheduled for a final virtual visit and again interviewed by a clinician.
The concordance between the self-assessment and the clinician assessment was high, showing agreement in 90.7% and 98.1% of cases at baseline and at the final treatment phase assessment, respectively. Participants also experienced a significant reduction in LDL cholesterol, which was reduced by 35.5%, on average, at six months from a baseline average of 140 mg/dL.
“Not only did participants self-select correctly, they also demonstrated they could appropriately selfadminister the drug and they obtained a reduction in LDL cholesterol that was about what you’d expect with high adherence,” Nissen said.
Researchers said previous efforts to make statins available without a prescription have encountered challenges ensuring that statins were truly appropriate for the people who were allowed to access them. In this study participants’ median 10-year risk of cardiovascular disease was estimated to be 10%, clearly placing them in a risk category for which statins are recommended.
No participants experienced serious adverse reactions to rosuvastatin during the study. One limitation of the web-based self-assessment approach is that it requires access to the internet, which could pose a barrier in some communities, Nissen said. The study was funded by AstraZeneca, maker of rosuvastatin.
For more information: www.acc.org


 July 31, 2024
July 31, 2024 









