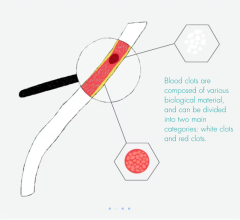
In patients with poor crural vessels assessed with angiographic runoff score, UPs were frequently detected in FPAs by angioscopy. Mural thrombi were more commonly observed on any of the UPs in patients with poor crural runoff. FPA = femoropopliteal artery; UP = ulcerated plaque. Image credit: T. Yamaguchi and T. Yamazaki
February 21, 2022 – A research group the Department of Cardiovascular Medicine, Osaka City University Graduate School of Medicine, has revealed for the first time that the thrombus generated by ulcerated plaque (UP) observed in the femoropopliteal artery (FPA) during angioscopy is the source of embolization of the popliteal artery. The results of this research are expected to help develop the best medical treatment for peripheral arterial disease (PAD).
In patients with PAD, the extent of infrapopliteal lesion is known to be an important factor correlating with prognosis. Recent pathological studies have suggested that embolization by an upstream thrombus is one of the mechanisms for the formation of infrapopliteal lesions, but the location where the thrombus occur in the body had yet been identified.
In a study of 31 patients who underwent endovascular therapy and angioscopy at the Department of Cardiovascular Surgery, Osaka City University Hospital, researchers identified 23 patients with irregular plaque buildup in the FPA, which they classified as UP. Angioscopic data showed 22 of these patients had mural thrombi in the FPA and on the UP - a ratio which was higher than in patients where no ulcerated plaque was observed. In addition, linear regression analyses revealed that UP was strongly correlated with the angiographic runoff score (ARS), an index reflecting the degree of occlusive stenosis in the popliteal artery. The results of this study were published online in the Journal of Vascular and Interventional Radiology on January 31, 2022.
“Previous reports used coronary artery findings to determine thrombus formation in the FPAs,” stated Tomohiro Yamaguchi MD, lead author of the study, “However, this creates complications due to critically different anatomical features among vessels between coronary arteries and FPA.”
From this study, the team observed that while the maximum yellow plaque color grade, taken from coronary artery findings, had no significant association with infrapopliteal ARS, the detection of UP was significantly associated with a poor ARS. This suggested a different mechanism for thrombus formation compared with that in the coronary artery.
“Although recent advances in catheterization for PAD have been remarkable, treatment results are still inadequate,” stated Dr. Takanori Yamazaki, who collaborated in the study. “We believe that a detailed assessment of the nature of plaque in femoropopliteal arteries, as found in this study, will help to explain the mechanism of the disease and develop optimal treatment methods.”
For more information: www.med.osaka-cu.ac.jp/e-index.shtml
Related Paclitaxel Safety Content:
No Increased Long-Term Mortality for the Paclitaxel-Coated Zilver PTX Stent
FDA Issues Letter About Paclitaxel Coated Balloons and Eluting Stents
Industry, Investigators Push Back With Patient-Level Data Showing No Increased Death From Paclitaxel-Based PAD Therapies
No Increased Long-Term Mortality for the Paclitaxel-Coated Zilver PTX Stent
FDA Issues Letter About Paclitaxel Coated Balloons and Eluting Stents
Top 10 Takeaways on Interventional Technologies at TCT 2020
No Mortality Risk Associated With Paclitaxel-coated Devices Used to Treat Peripheral Artery Disease
FDA Panel Recommends Continued Use of Paclitaxel-coated Peripheral Devices
Safety of Paclitaxel-eluting Stents and Balloons Called Into Question
6 Hot Topics in Interventional Cardiology at TCT 2019


 September 12, 2025
September 12, 2025