Diagnostic & Invasive Cardiology editor Kim Phelan spoke with Jeff Mirviss, vice president of Stent Marketing at Boston Scientific to get a first-hand perspective and highlights from the FDA panel that reviewed the safety of drug-eluting stents on Dec. 7 and 8. Following are excerpts from that phone interview Dec. 12.
Outline what you consider to be the key highlights from the two-day meeting.
It appears that the panel was quite comfortable with the relative net clinical benefit of drug-eluting stents in that the safety was viewed as equivalent to bare metal stents, yet there was a significant and profound clinical benefit in terms of reducing the need for a second procedure. That discussion was centered primarily around the on-label indications where we have a very robust set of data in our randomized clinical trial.
Look at the type of endpoints that patients really care about the most: (1) Am I going to be alive at a certain point of time in the future? and (2) Am I going to have a major heart attack? If you look at those two endpoints, death and MI, there was essentially no difference between bare metal stents and drug-eluting stents. That is why I think there was a lot of discussion around the net clinical benefit or the risk benefit of drug-eluting stents — there is no difference in safety yet you get this benefit in terms of reducing the need for a second procedure.
Interestingly enough, if you look at the Taxus data, there is actually a trend toward a benefit for both death and MI. So we were quite pleased with the discussion and the way that the FDA framed it up.
Then, when they looked at some of the subsets such as diabetics, patients with very small vessels, patients with really long lesions, or patients who have multiple stents in a procedure, what the data showed was that the benefit in terms of reducing the need for a second procedure was profoundly there in all of those subsets.
And as you look at more complex patients, you see that the bare metal stent actually started to degrade even more in performance for second procedures, yet the safety was very similar in the randomized data.
Lastly, looking at the stent thrombosis rate in particular, I think that you also saw the panel and the subsequent media pick up on the fact that there is enough data support that late stent thrombosis is a class effect — it occurs in both of the commercially available drug-eluting stents as well as release of the data from Medtronic so far. So there is a signal there in terms of late stent thrombosis, but again, the net benefit of those differences in death and MI is supporting the fact that these products are safe.
Describe the nature of the discussion related to Clopidogrel, aka dual anti-platelet therapy. How did the panel weigh in on that side of the issue?
The end conclusion was that there isn’t enough definitive data to make a formal labeling change. They did feel that there was enough data to suggest that what the AHA and ACC recommend should be put in the manufacturer’s label so that patients and clinicians can be aware, or more aware of what AHA and ACC recommendations are, essentially that: in complex patients who can tolerate longer term dual anti-platelet therapy, they should consider prescribing it longer in most patients.
[Boston Scientific] did an analysis within the Taxus data showing (and there was other data at the panel to support this as well) that in these complex patients, longer term Plavix actually had a reduced death rate compared to bare metal stents. I think there is also some Plavix data suggesting that longer term Plavix in some patients is better — but there is not enough definitive data to say for which patients and for how long.
There was some dialogue back and forth between the panel members about whether we should just inform physicians and patients and let physicians make the decision, or whether we should mandate something. They concluded that there is not enough data to mandate anything — let’s just make sure that the information is available.
Boston Scientific is finishing enrollment on two additional randomized trials — will either look at the anti-platelet aspect in any way?
Yes and no. They were not designed to prospectively look at different rates of dual anti-platelet therapy, but I’m sure there will be, as there are in other Taxus trials, patients who will be taking meds for varying times and we will do some type of an analysis after the trial to look at these differences.
What about the announcements we heard at TCT in which the manufacturers will collaborate on studies of some 50,000 patients? Where does that stand?
Each of the competitors has announced some sort of trial to look at the issue of late stent thrombosis or Plavix. What we announced was the Stent Thrombosis Registry with Dr. Chuck Simonson. Gregg Stone is also going to be the PI of this Stent Thrombosis Registry, and this will be 10,000 patients with long-term follow up in the real world, to try and understand in greater detail the causes of late stent thrombosis. There will be a host of matrices looked at to inform us on which patients are at risk for thrombosis and how do we prevent that risk going forward.
A lot of our product development pipeline is aimed at increasing the safety and efficacy of drug-eluting stents. We have a large effort underway that will get after the issue, and the Stent Thrombosis Registry will help to inform that product development effort.
Were there any surprises during the FDA meeting? Anything that you were not expecting?
I wasn’t expecting the strong point of view by a few panel members — and it was the minority — as to the strong advocacy for bypass surgery. I think the benefits of percutaneous therapy and a minimally invasive approach so far outweigh a surgical approach. I didn’t think that it would go down the path of: “Maybe we should be doing surgery on any off-label patient.” I think that was an extreme view, but it did surprise me that there was a discussion around the role of bypass surgery in today’s treatment of coronary artery disease.
What is your sense of what will come next, in terms of any FDA action or decision-making.
This is my opinion, because obviously nobody knows, but I believe that they are going to come out at some point in the near future with a statement, similar to what they did not too long ago, posting a statement on drug-eluting stents on their Web site. I believe the statement will be aimed at alleviating patients’ uncertainty and clarifying the issues around drug-eluting stents. I think they will strongly endorse that they are safe and significantly more effective than bare metal stents for on-label indications. For these patients they are a good choice for coronary artery disease treatment, and more data is needed in off-label patients. Physicians should weigh the risks and benefits in patients where there is not enough data yet to make a definitive conclusion — at the end of the day, it is up to the patient and their physician. In cases of these complex patients there is some data that suggests that long-term Plavix may be more beneficial to reduce some of the hard end points such as death and MI, and I think FDA will leave it in the hands of the interventional cardiologist and then follow up at some point in the future with another panel reading.
There were a lot of kind of comments like, “This is a really good meeting and I think we should do it more often.” I think that once a year, in a market that affects as many patients as this one does, it wouldn’t be so terrible to have some sort of [periodic] overseeing to discuss these issues.
Lastly I think that the FDA is going to raise the bar in terms of the information and data that they are going to need to approve these drug-eluting stents for all of us, including Boston Scientific. They are going to be more diligent in their analysis of the data, the analysis of the information that we provide from manufacturing and bench testing. Then they are going to be more disciplined in ensuring that companies follow their commitment, more diligent in holding the industry accountable.
Any final thoughts?
I would just reiterate that we are extremely confident in our data; we have taken a philosophy of full transparency, and we are communicating broadly to our customer base the same information that we have communicated to FDA.
At the end of the day, for patients who are receiving drug-eluting stents, the data strongly supports that there is an enormous clinical benefit for reducing the chance for a second procedure, And with Taxus, there is even a trend toward less death and MI than bare metal stents. So we believe this is the best choice for patients — we think the data supports it, we are encouraged by the FDA statements, and we look forward to continuing to provide the market with the excellent technology in the Taxus program.
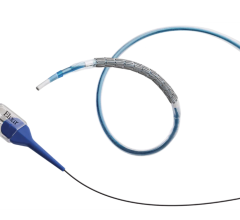
As we look forward to ’07 and beyond, we have numerous new technologies that we are on cusp of launching. We are expanding the current Taxus product to provide clinicians with more stent lengths and diameters. We have a brand new stent in the Taxus Liberte that will improve deliverability, and we have a whole second drug platform in everolimus that we’re calling Promus.
We are confident in the future of drug-eluting and we really believe in the safety.


 July 02, 2024
July 02, 2024