Courtesy Getty Images
November 18, 2021 — Adults undergoing mitral valve surgery who have less than severe leakage of the tricuspid valve may benefit by having both valves repaired at the same time, including a decreased chance of severe tricuspid valve leakage in the future, according to late-breaking research presented at the American Heart Association’s Scientific Sessions 2021. The CTCR-MVS study evaluated the benefit of concomitant tricuspid repair during mitral valve surgery.
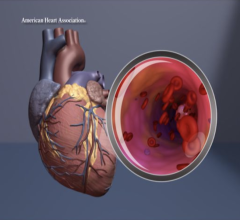
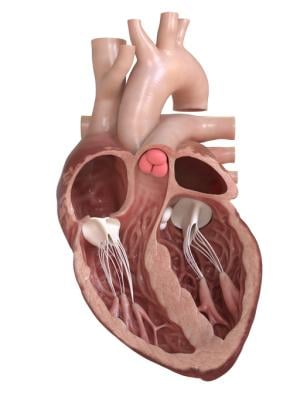
Heart valves are responsible for regulating blood flow to and from the chambers of the heart. The four valves of the heart all have leaflets, or cusps, which work to open and close so blood can flow through the heart, while also preventing blood from flowing backwards. Mitral valve regurgitation (leakage) is the most common reason for cardiac surgeons to perform surgery to either repair or replace the mitral valve. A leaky mitral valve often leads to tricuspid valve regurgitation. Leakage of the tricuspid valve is graded using ultrasound as none, mild, moderate and severe. Experts generally recommend that a patient with a severely leaky tricuspid valve who is having mitral valve surgery should have the leaky tricuspid valve repaired at the same time.
“While there is general agreement that a severely leaky tricuspid valve should be fixed when a surgeon is operating on the mitral valve, there is considerable uncertainty as to whether to fix the tricuspid valve when the leakage is only moderate or less,” said lead investigator James S. Gammie, M.D., the James T. Dresher Sr., professor of Cardiac Surgery and surgical lead and co-director of the Johns Hopkins Heart and Vascular Institute at Johns Hopkins University in Baltimore. “Repairing the tricuspid valve may confer benefit by preventing the development of significant leakage over time, which can cause damage to the heart. There are also potential disadvantages. The operation will take longer, which could increase complications and risk, and tricuspid valve repair increases the risk of patients needing a permanent pacemaker. Contemporary practice patterns are quite varied and reflect this uncertainty.”
To evaluate the potential effectiveness and safety of tricuspid valve repair during mitral valve surgery when tricuspid regurgitation was moderate or less than moderate, researchers conducted an international, multicenter randomized controlled trial at 39 centers across the U.S., Canada and Germany between 2016 and 2018. A total of 401 adults were included in the study: 203 patients had only the mitral valve operation, while 198 patients had mitral valve surgery plus tricuspid valve repair. The participants were primarily white men (91% white; 75% were men) and had an average age of 67 years. Researchers assessed the rate of death, repeat operation for tricuspid regurgitation and progression of tricuspid valve leakage.
Study researchers conducted a two-year follow-up on all study participants. Overall, the participants who had both their mitral valve and their tricuspid valve repaired experienced better outcomes than those who had only their mitral valve repaired.
The analysis of all study participants found:
- Only 0.6% of the participants in the mitral valve plus tricuspid valve surgery group had progressed to severe tricuspid regurgitation after two years, compared to 5.6% of those in the mitral valve-only surgery group.
- The difference in the number of study participants who progressed to either moderate or severe tricuspid regurgitation was significant. Only 3.4% of people who had both valves repaired had moderate or severe tricuspid regurgitation after two years, compared to about 25% of those who had the mitral valve surgery alone.
- The addition of tricuspid valve repair to the mitral valve surgery did prolong the amount of time patients spent on the heart-lung machine by 34 minutes.
- Pacemakers were needed in the tricuspid valve repair group significantly more often (14.1%) than in the mitral valve-only surgery group (2.5%). The researchers noted the need for the pacemaker did not appear to have a negative impact on patients.
- The difference in tricuspid regurgitation in the two groups had no impact on survival, heart function, symptoms or quality of life.
“This trial highlights the safety of modern mitral valve surgery. The mortality rate for people in this study was less than 1%, and two years later more than 96% of patients had survived,” Gammie said. “While the differences in tricuspid regurgitation and pacemaker implantation were of great interest, they didn’t seem to have an impact on survival, quality of life or cardiac function. We clearly need to better understand the risk factors for needing a permanent pacemaker implanted after tricuspid valve repair, and how to best mitigate this risk. That may entail technique modifications and/or changing post-operative management strategies.”
Gammie noted it is important for surgeons to discuss all options with their patients to determine which strategies are optimal for those who needs mitral valve surgery, and whether tricuspid valve disease should be addressed at the same time.
“This trial demonstrates the power of an incredible collaboration and hard work on the part of the research teams across North America, as well as in Germany,” Gammie said. “It will be crucial to continue to follow this study group to see what the impact of tricuspid progression has on clinical and cardiac function parameters over an extended time.”
Co-authors are Michael W Chu, M.D.; Peter K. Smith, M.D.; Jessica R. Overbey, Dr.Ph.; Michael J. Mack, M.D.; Pierre Voisine, M.D.; Markus Krane, M.D.; A. Mark Gillinov, M.D.; Michael E. Bowdish, M.D.; Lenard Conradi, M.D.; Steven F. Bolling, M.D.; Marissa A. Miller, D.V.M., M.P.H.; Wendy C. Taddei-Peters, Ph.D.; Neal O. Jeffries, Ph.D.; Mariell Jessup, M.D., FAHA; Eric A. Rose, M.D.; John C. Mullen, M.D.; Samantha Raymond, M.P.H.; Ellen G. Moquete, B.S.N.; Karen O’Sullivan, M.P.H.; Mary E. Marks, B.S.N.; Alexander Iribarne, M.D., M.S.; Friedhelm Beyersdorf, M.D.; Michael Andrew Borger, M.D., Ph.D.; Arnar Geirsson, M.D., FAHA; Emilia Bagiella, Ph.D.; Judy Hung, M.D.; Alan J. Moskowitz, M.D.; Annetine C. Gelijns, Ph.D., J.D.; Patrick T. O’Gara, M.D.; Gorav Ailawadi, M.D.; and Volkmar Falk, M.D. Authors’ disclosures are listed in the abstract.
The trial was funded by a cooperative agreement by the National Heart, Lung, and Blood Institute of the National Institutes of Health and a grant from the German Centre of Cardiovascular Research.


 November 14, 2025
November 14, 2025