
May 5, 2016 — Intact Vascular Inc. announced that positive twelve-month results from its Tack Optimized Balloon Angioplasty – Below-the-Knee (TOBA-BTK) clinical study were presented at the SCAI 2016 conference. Results were presented by Dr. Christian Wissgott, assistant director at Westküstenklinikum Heide in Heide, Germany.
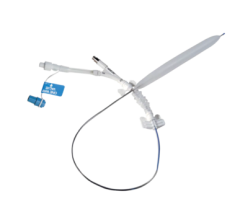
The TOBA-BTK study enrolled 35 subjects at six sites in Europe and New Zealand. All study subjects were suffering from critical limb ischemia, a form of peripheral arterial disease, in one or both legs. Of the subjects enrolled, 32 were treated with the 4 French Tack Endovascular System following standard balloon angioplasty in the tibial and peroneal arteries. The Tack Endovascular System is a new technology designed to repair dissections (or tears) in the artery wall that frequently occur as a complication of balloon angioplasty. The system allows physicians to repair these dissections while leaving a minimal amount of foreign material in the artery, reducing mechanical stress on the artery, and preserving future treatment options.
Some of the key conclusions from the TOBA-BTK study included:
- 78.4 percent 12-month primary patency;
- 89.2 percent 12-month primary assisted patency;
- 93.5 percent freedom from target lesion revascularization (TLR);
- 84.5 percent amputation-free survival; and
- 87.1 percent freedom from major amputation.
Wissgott stated, “Restoring blood flow to the legs in patients with critical limb ischemia is vitally important to their quality of life and survival. We have few treatments that have a demonstrated ability to keep the small arteries below the knee open over 12 months, so these TOBA-BTK results are truly encouraging. These data suggest that repairing arterial dissections following angioplasty below the knee, using the minimal metal design approach of the Tack implant, can keep the treated arteries open and blood flowing.”
Patients in the study demonstrated a marked improvement as measured by the Rutherford Classification System, a seven-stage scale ranging from no symptoms (class 0) to gangrene (class 6). The study data suggest that an increasing number of patients continue to improve, with 75 percent of patients experiencing a four- or five-step improvement in Rutherford Classification from baseline (p<0.0001) at 12 months.
Wissgott continued, “The Tack Endovascular System holds much promise for improving the long-term outcomes associated with balloon angioplasty below the knee. I look forward to building on these exciting results in the expanded TOBA II BTK clinical trial that is currently being planned.”
Based on these results, the company is pursuing an expanded study (TOBA II BTK) that will assess the performance of the Tack Endovascular System in a larger population and will include U.S. and international investigators.
For more information: www.intactvascular.com

 June 13, 2024
June 13, 2024 









