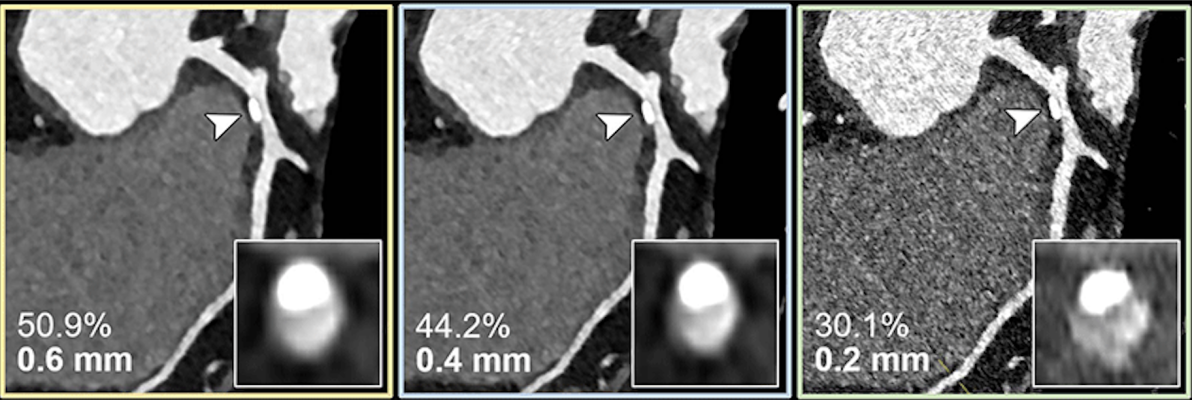
Coronary CT angiography for the suspected progression of known coronary artery disease in a 56-year-old female patient. Curved multiplanar reconstructions with 0.6-mm (yellow outline), 0.4-mm (blue outline), and 0.2-mm (green outline) section thickness show the respective calcified plaque (arrowheads) and coronary stenosis (inset images). The reduced section thickness leads to less calcium blooming and therefore a less severe assessment of percentage of coronary stenosis in this patient.
https://doi.org/10.1148/radiol.231956 © RSNA 2024
February 20, 2024 — Ultrahigh-spatial-resolution photon-counting detector CT improved assessment of coronary artery disease (CAD), allowing for reclassification to a lower disease category in 54% of patients, according to a new study published today in Radiology, a journal of the Radiological Society of North America (RSNA). The technology has the potential to improve patient management and reduce unnecessary interventions.
Coronary CT angiography is a first-line test in the assessment of coronary artery disease. However, its diagnostic value is limited in patients with severe calcifications, or calcium buildup in the plaque of the coronary arteries.
Ultrahigh-spatial-resolution photon-counting detector CT (PCD-CT) improves image quality compared to conventional CT. Additionally, it provides better spatial resolution, or the ability to differentiate two adjacent structures as being distinct from one another.
“Our study provides a glimpse into the potential impact of performing coronary CT angiography using ultrahigh spatial resolution technology on risk reclassification and recommended downstream testing,” said study co-author Tilman Emrich, M.D., attending radiologist at the University Medical Center Mainz in Germany, and assistant professor of radiology at the Medical University of South Carolina in Charleston.
For the study, researchers evaluated coronary stenoses, or narrowing in the coronary arteries, in a vessel phantom (in-vitro) containing two different stenosis grades (25%, 50%), and retrospectively in 114 patients (in-vivo) who underwent ultrahigh-spatial-resolution cardiac PCD-CT for the evaluation of coronary artery disease. In-vitro values were compared to the phantom’s manufacturer specifications, and patient results were assessed regarding effects on coronary artery disease reporting and data system reclassification (CAD-RADS).
“The study used a combination of artificial vessel models and real-world patient data,” Dr. Emrich said. “It simulated three types of reconstructions from a single PCD-CT scan, resembling conventional CT, high-resolution, and ultrahigh-spatial-resolution scans. Observers evaluated the severity of stenosis and generated CAD-RADS classifications, guiding further patient management decisions.”
In-vitro results demonstrated a reduced overestimation of the stenosis by ultrahigh-spatial-resolution scans by reducing the adverse effects of the calcifications on the image.
Results from the patients with suspected or diagnosed coronary artery disease confirmed a lower median degree of stenosis for calcified plaques (29% vs. 42%) with ultrahigh-spatial-resolution PCD-CT compared to standard CT. Ultrahigh-spatial-resolution often led to patients being reclassified to a lower CAD-RADS category. Of the 114 patients, 54% were given a lower CAD-RADS classification than they were originally assigned. The researchers found in-vitro quantification of the 193 coronary CT angiography-based stenoses was also more accurate using ultrahigh-spatial-resolution than standard resolution.
“We found that ultrahigh-spatial-resolution reconstructions resulted in significant changes in recommendations for over 50% of patients,” Dr. Emrich said. “The impact was particularly notable in cases with calcified plaques, where ultrahigh-spatial-resolution reduced the overestimation of stenosis.”
Dr. Emrich explained that ultrahigh-spatial-resolution may address the current limitations of conventional cardiac CT angiography by reducing the overestimation of stenosis due to calcium blooming, an effect which can cause small, high-density structures—such as calcifications—to appear larger than their true size.
“This could significantly alter recommendations for downstream testing, potentially leading to a reduction of unnecessary procedures (and their potential complications) and reduced healthcare costs,” he said.
No substantial benefits of ultrahigh-spatial-resolution were observed for mixed and non-calcified plaques.
“It is important to note that these findings are from a simulation study, and further validation is needed in real-world comparisons,” Dr. Emrich said.
For more information: www.rsna.org


 October 08, 2025
October 08, 2025