Getty Images
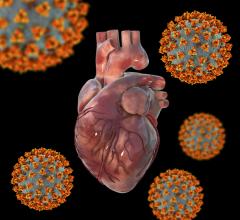
May 11, 2021 — Patients hospitalized with COVID-19 may be at risk of developing heart failure even if they do not have a previous history of heart disease or cardiovascular risk factors, a new Mount Sinai study shows.
Researchers say that while these instances are rare, doctors should be aware of this potential complication. The study, published in the April 26 online issue of the Journal of the American College of Cardiology, may prompt more monitoring of heart failure symptoms among patients hospitalized with COVID-19.
“This is one of the largest studies to date to specifically capture instances of new heart failure diagnosis among patients hospitalized with COVID-19. While rare, the finding of new heart failure was more common among patients with preexisting cardiovascular risk factors or disease. But there were select individuals who developed new heart failure without risk factors or disease. We need to learn more about how SARS-CoV-2 [the virus that causes COVID-19] may directly affect the cardiovascular system and precipitate new heart failure- as to whether it is an indirect effect of critical illness or direct viral invasion,” said lead researcher Anu Lala, M.D., Director of Heart Failure Research at the Icahn School of Medicine at Mount Sinai. “Importantly, though symptoms of heart failure—namely shortness of breath—can mimic symptoms associated with COVID-19, being alerted to the findings of this study may prompt clinicians to monitor for signs of congestion more consistent with heart failure than COVID-19 alone.”
The team of researchers looked at electronic medical records of 6,439 admitted and confirmed COVID-19-positive adult patients between February 27 and June 26, 2020, at Mount Sinai Health System hospitals. The median age was 64. Investigators found 37 patients (0.6 percent) with no prior history of heart failure who developed new cases of heart failure during their hospitalization for COVID-19. Of those new heart failure patients, eight of them (22 percent) had no previous cardiovascular disease or risk factors, while 14 had a history of heart disease and 15 had no heart disease but at least one risk factor for it. The eight patients with no prior history were younger with an average age of 43, mostly male, and had lower body mass index and fewer comorbidities such as respiratory or renal diseases. These eight patients also had more instances of cardiogenic shock, a life-threatening condition where the heart suddenly can’t pump enough blood to the body. The patients who did have a history or risk factors for heart disease were, on average, 73 years old. All new heart failure patients were in the hospital for a similar amount of time, seven days on average, and survival rates were similar among both groups.
“Understanding specific mechanisms as to how COVID-19 may precipitate new heart failure should be the focus of future work,” said first author Jesús Álvarez García, M.D., Ph.D., a postdoctoral fellow in advanced heart failure and transplantation at Icahn Mount Sinai.
“Moving forward, we also need to monitor patients after hospitalization for COVID-19 for signs and symptoms of heart failure, based on studies demonstrating fibrosis in the myocardium on MRI following infection. We still need to understand underlying mechanisms of injury related to infection with SARS-CoV-2. It has become obvious that the pandemic and its aftermath will be with us for some time, so devoting energy to better understanding its impact on the cardiovascular system, particularly as it relates to the precipitation of heart failure, is crucial,” said Lala. “It will also be important to monitor if patients develop heart failure later down the line, and more broadly how the cardiovascular system is impacted after recovery from COVID-19.”
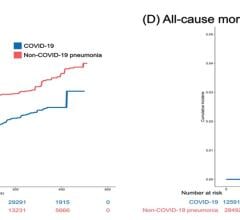
This study is an extension of previous Mount Sinai research that found patients with a history of heart failure and hospitalized with COVID-19 were more likely to experience a longer hospitalization, nearly three times the risk of intubation and mechanical ventilation, and double the risk of death, compared to those without a history of heart failure.
For more information: www.mountsinai.org

 March 20, 2024
March 20, 2024