February 9, 2009 - Implantation of drug-eluting stents to treat degenerative in aortocoronary saphenous vein graft (SVG) lesions is safe, according to a study published in the Jan. 15 issue of the American Journal of Cardiology (Vol. 103, issue 2, Pages 199-202).
The Paclitaxel-Eluting Stent Long-Term Outcomes in Percutaneous Saphenous Vein Graft Interventions (PELOPS) Study by researchers at the Cardiac Medical Unit of Grantham Hospital and the Department of Medicine at Queen Mary Hospital, both in Hong Kong, said paclitaxel-eluting stents in SVGs showed an association with low late loss, angiographic restenosis, and MACE at one-year follow-up.
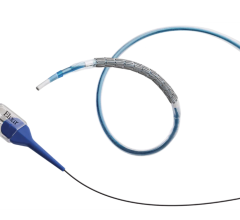
Sixty-eight consecutive patients with 90 nonoccluded SVG lesions were treated with a Taxus stents ranging in size from 2.25 to 4.5 mm. Angiographic follow-up was performed on 63 patients (93 percent) and 83 lesions (92 percent) at 12 months. Researchers said major adverse cardiac event (MACE) was recorded in all patients at one year. The mean age of patients was 71 with predominance of men (75 percent). Glycoprotein IIb/ IIIa inhibitors were given in 21 patients (31 percent). Embolic protection devices were used in 54 lesions (60 percent). On average, patients received 1.4 stents per lesion with a stent size of 3.4 ± 0.6 mm and a length of 35.8 ± 27 mm.
Angiographic follow-up revealed a late loss of 0.36 ± 0.66 mm with an in-segment binary restenosis rate of 7 percent. The in-hospital MACE was 7 percent, which was solely contributed by 5 patients with postprocedure non–Q myocardial infarction. The one-year MACE was 15 percent, accounted by one noncardiac death and nine patients with target vessel revascularization. Peripheral vascular disease and the use of glycoprotein IIb/ IIIa inhibitors were the independent predictors of MACE at one year, the researchers said.
For more information: www.ajconline.org


 July 02, 2024
July 02, 2024