July 27, 2017 — There is good news when it comes to the heart’s sinoatrial node (SAN), the body’s natural pacemaker. Scientists at The Ohio State University Wexner Medical Center have shown the human SAN is hardwired with a backup system — three diverse regions of pacemakers acting as batteries and up to five conduction pathways that act as wires to connect the signal to the atria. This built-in redundancy maintains consistent heart rhythm, even under trying conditions.
The research is published online by the journal Science Translational Medicine.
Like a battery, the SAN generates electrical impulses to initiate heartbeats. Until now, scientists didn’t know for sure how the SAN protected the heart’s rhythm and how the system failed.
“It’s been challenging because our human SAN differs greatly from well-studied animal models, and clinical electrode recordings only capture what’s on the surface,” said Vadim Fedorov, an associate professor in Ohio State’s Department of Physiology and Cell Biology.
So Fedorov and his team applied optical mapping, 3-D structural imaging and molecular mapping to 21 explanted human hearts to define the internal function of the SAN. The hearts, which are not viable for human transplant, were donated by heart transplant recipients and Lifeline of Ohio.
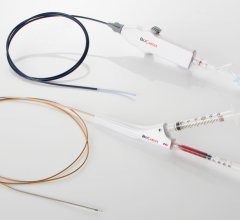
To resuscitate the hearts, researchers placed them in a glass chamber filled with an oxygenated solution at body temperature and perfused the coronary arteries with warm, oxygenated solution that simulates blood flow, allowing the SAN to beat again with the same rhythm as when it was inside the body for at least 12 hours.
Then the chamber with live heart tissue is surrounded by four highly-sensitive infrared cameras, and a fluorescent dye is injected. This dye can visualize spontaneous electrical activity moving within the human SAN in 3-D.
“We observed that all three intranodal pacemakers are used, depending on the heart’s needs at rest, or during normal or high exertion,” Fedorov said.
To study how the SAN functions under stress, Fedorov’s team applied adenosine, a heart rhythm regulator that is overproduced when there is heart failure and inadequate blood supply.
“The central pacemaker was most affected, as it is highly sensitive to adenosine. The head and tail pacemakers were able to maintain a slower rhythm and prevent complete cardiac arrest. We saw similar shifts in the preferred conduction pathways,” Fedorov said. Total cardiac arrest occurs only when all pacemakers or conduction pathways fail, whether due to disease or age.”
When there is a problem with SAN pacing or conduction, doctors implant an electronic pacemaker to prevent cardiac arrest. Approximately 225,000 Americans get a pacemaker every year, according to the World Society of Arrhythmia.
“Patients are at high risk of cardiac arrest if the SAN gets down to one pacemaker, or one conduction pathway,” Fedorov said. “Knowing this, our next quest is to work with electrophysiologists to more precisely identify who needs a pacemaker implant, and who still has backups and can get along without one.”
Clinicians are excited by this discovery.
“It’s groundbreaking. This is the first step in explaining why the SAN can be ‘sluggish’ for years before a total failure, allowing the clinician to detect the problem before a catastrophic event,” said Raul Weiss, M.D., a cardiologist and clinical researcher at Ohio State.
“I think this work can fundamentally change the way we diagnose disease of the heart’s natural pacemaker,” said John Hummel, M.D., a cardiologist and clinical researcher at Ohio State. “In some patients, it can be incredibly challenging, and these insights may allow us to diagnose those challenging patients more effectively.”
Because a pacemaker is merely a crutch and cannot fix the underlying problem, Fedorov’s team is also seeking out ways to improve or restore the impaired portions of the SAN. Their hope is that someday, pacemaker implants could be obsolete.
This research was funded by the National Institutes of Health, the American Heart Association, the C.R. Webb Fund in Cardiovascular Research and the TriFit Challenge Discovery Fund.
Other Ohio State researchers include: Ning Li, Brian Hansen, Thomas Csepe, Anthony Ignozzi, Lidiya Sul, Stanislav Zakharkin, Anuradha Kalyanasundaram, Jonathan Davis, Brandon Biesiadecki, Ahmet Kilic, Paul Janssen and Peter Mohler.
For more information: www.stm.sciencemag.org


 January 29, 2026
January 29, 2026