Getty Images
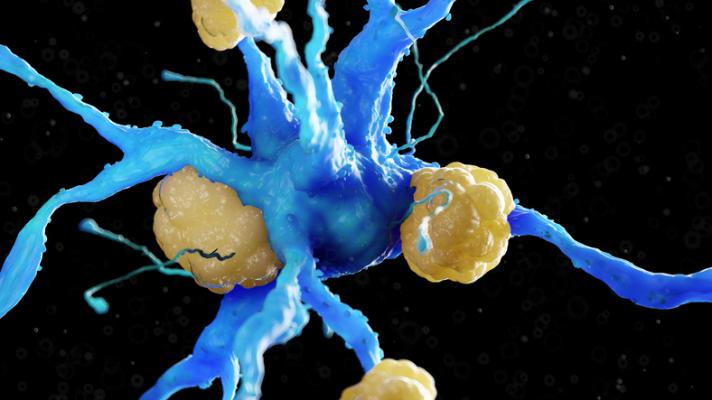
June 7, 2024 — Calcific aortic valve disease (CAVD) is the major heart valve disease that afflicts nearly 10 million patients globally with an annual mortality exceeding 100,000, and the numbers continue to rise. In CAVD, microcrystals of hydroxyapatite (a calcium phosphate mineral) deposit onto the heart valve leaflets and impair cardiac function. The disease has a dismal prognosis with most untreated patients dying two years after diagnosis. Currently, the only available treatment is surgical aortic valve replacement, which is not appropriate for all patients.
While previous studies of the histology samples from explanted calcified aortic valves have found amyloid deposits in or near calcified areas, the causal relationship between amyloid deposition and calcification is unclear.
Researchers from Boston University Chobanian & Avedisian School of Medicine, in collaboration with clinical cardiologists from New York University and University of Texas Houston, have now proposed a molecular mechanism that links amyloid deposition in the aortic valve with degenerative calcification. They also theorize that other risk factors for CAVD, such as high blood levels of lipoprotein, can contribute to calcification both directly and indirectly through the mechanisms that involve amyloid accumulation.
Harnessing the “resolution revolution” in cryogenic electron microscopy, groups of researchers around the world were able to determine hundreds of structures of patient-derived protein aggregates called amyloid fibrils. Such fibrils are associated with major human diseases including Alzheimer’s and Parkinson’s diseases, diabetes, and heart diseases such as atherosclerosis and calcific aortic valve disease. “We noticed that the unique geometry of amyloid fibrils, with their periodic arrays of acidic residues on the surface, provides a perfect match for the precursors of calcium phosphate crystals that deposit in the heart valve and impair its normal function,” explained corresponding author Olga Gursky, PhD, professor of pharmacology, physiology & biophysics at the school.
The researchers propose that amyloid deposits, which are often found adjacent to calcified areas of the heart valve, can modulate CAVD and accelerate degenerative calcification. This implies that blocking amyloid formation may be a much-needed novel therapeutic target for CAVD and, potentially, other diseases involving degenerative calcification and amyloid formation, such as Alzheimer’ disease.
“We hope that a better understanding of molecular mechanisms and drivers of degenerative biomineralization will help identify new therapeutic targets for major human diseases, such as calcific aortic valve disease,” adds Gursky.
These findings appear online in the journal Trends in Molecular Medicine.
For more information: https://www.cell.com/trends/molecular-medicine/home


 January 05, 2026
January 05, 2026 









