July 8, 2009 – A procedure that sends targeted energy into the heart through a catheter can be used to treat a common type of irregular heartbeat, but little is known about the treatment's long-term benefits and the best methods and circumstances for applying it, according to a new report funded by the Health and Human Services' (HHS’) Agency for Healthcare Research and Quality (AHRQ).
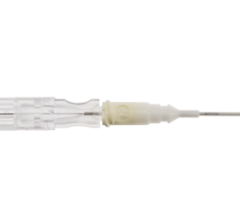
The report examines the use of a procedure called radiofrequency catheter ablation to treat atrial fibrillation (AF). The new comparative effectiveness report found the procedure can provide benefits in maintaining normal heart rhythm over short periods of time (up to one year), but found little evidence indicating whether the procedure reduces the chance patients will experience AF over the long term.
The report, which compared radiofrequency (RF) catheter ablation to medication-based therapy, also found that the effect of the procedure on stroke, a major risk for patients with AF, is unknown.
There is little evidence indicating the procedure's effectiveness when used as a first-line therapy instead of medication.
"Radiofrequency holds promise for treating atrial fibrillation, but it is clear that more research is needed to demonstrate its potential long-term benefits," said AHRQ Director Carolyn M. Clancy, M.D. "This report crystallizes the questions that researchers need to ask going forward."
The report calls for more research on the effect of radiofrequency catheter ablation on quality of life. In particular, more research is needed for groups of patients for whom the research is especially lacking, such as women, the elderly and patients who have other conditions such as heart failure or high blood pressure.
Earlier this year, HHS' FDA approved the first two ablation catheters indicated for use in treating atrial fibrillation in the U.S. However, physicians often use other catheters not approved by the FDA for atrial fibrillation. The FDA also found there is no conclusive evidence that people whose symptoms are reduced with ablation are less likely to have a stroke. Therefore, the FDA explicitly endorsed existing clinical guidelines that recommend patients at-risk for stroke continue to take preventive blood-thinning medications after radiofrequency catheter ablation.
As a condition of catheter approvals, the FDA mandated the catheters' manufacturer must conduct two post-approval studies (PAS) to collect long-term safety data. The mandated studies apply only to FDA-approved catheters, and not to devices used off-label in clinical practice. The first PAS is a post approval registry, which will collect safety (adverse event) data and operator experience information through seven days post-treatment with the approved ablation catheters. The study will also collect long term safety (adverse events) data, such as death, stroke, myocardial infarction, clinically manifested pulmonary vein stenosis, etc., at five years post-treatment. The second PAS is a subgroup analysis from an ongoing larger study that will look at the incidence of stroke, and compare the three-year incidence of stroke between patients treated with the approved ablation catheters versus patients treated with medication. This study will analyze total mortality, serious bleeding and cardiac arrest.
AHRQ's new report, “Comparative Effectiveness of Radiofrequency Catheter Ablation for Atrial Fibrillation,” is the newest analysis from the agency's Effective Health Care Program.
For more information: www.effectivehealthcare.ahrq.gov


 October 28, 2025
October 28, 2025