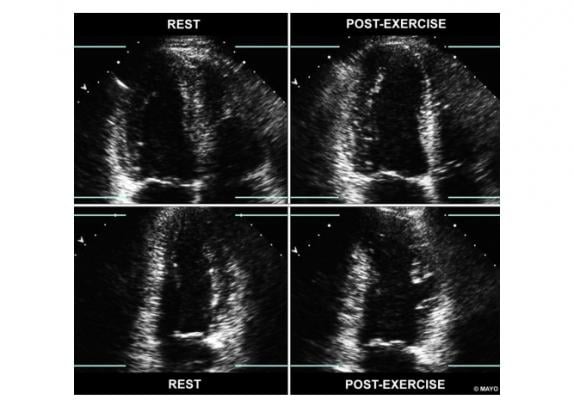
Figure 1 from the guidelines, showing a side-by-side views of apical 4- and 2-chamber images, at rest and immediately post-exercise. In the four-chamber view, the left ventricle is shown on the left-hand side of the screen. With exercise, the LV cavity dilates (right quadrants) and there are regional wall motion abnormalities in the LAD territory.
January 7, 2020 — The American Society of Echocardiography (ASE) has updated its guidelines for using echocardiography to image ischemia. Ischemic heart disease (IHD) occurs when the arteries of the heart cannot deliver enough oxygen-rich blood to the heart and is the leading cause of death in the United States. Stress echocardiography is routinely used for the detection of flow-limiting blockages in the coronary arteries in patients with symptoms such as exertional chest pain or shortness of breath. In this era of multimodality imaging, understanding the role and advantages of stress echocardiography for the patient presenting with symptoms of potential cardiac origin is essential.
The "Guidelines for Performance, Interpretation, and Application of Stress Echocardiography in Ischemic Heart Disease: From the American Society of Echocardiography," replaces the 2007 ASE guideline on stress echocardiography.[1] The older guidelines did not include class of recommendation and level of evidence, which are now included in this updated document, in addition to current practice recommendations and training requirements.
“Stress echocardiography is appropriate for evaluation of the patient presenting with symptoms of suspected ischemic heart disease," said the ASE’s Chair of the writing group, Patricia Pellikka, M.D., FACC, FAHA, FASE, of Mayo Clinic in Rochester, Minn. "In addition to detecting ischemia, stress echo can reveal diastolic dysfunction, pulmonary hypertension, valvular disease, and other cardiac causes of symptoms. Stress echo is also useful in periodic assessment of children at risk of ischemia, such as those who have undergone heart transplant or with Kawasaki Disease. Exercise stress echocardiography is particularly well-tolerated by all patients who can exercise.”
She added, “Comparative studies of stress echocardiography versus other modalities have not taken into account the incremental value of the ancillary findings detected by echocardiography at the time of stress echocardiography, including detection of non-ischemic causes of cardiac symptoms.”
The current guidelines include new recommendations regarding quantitative analysis of stress echocardiography, including assessment of myocardial deformation with speckle tracking.
In conjunction with the publication of this guideline, Pellikka will conduct a live webinar, including a question and answer section, on Wednesday, Feb. 5, 2020, at 1 p.m. Eastern time. The webinar will be available for free to all ASE members and open to all other clinicians for $25. Registration and access to all ASE-hosted guideline webinars are available on ASEUniversity.org.
The full guideline document is available on the Journal of American Society of Echocardiography (JASE) website OnlineJASE.com. This document and all ASE Guideline documents are also available to the medical community at ASEcho.org/Guidelines.
Reference:


 June 12, 2024
June 12, 2024 









