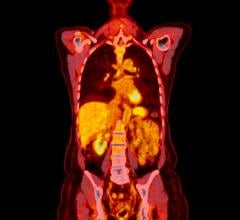
June 19, 2013 — Coronary artery disease (CAD) is one of the world’s most prevalent and silent killers. Positron emission tomography (PET), which images miniscule abnormalities in cellular metabolism, can tip off clinicians about cardiac disasters waiting to happen — including sudden death from a heart attack — better than standard angiography, researchers revealed at the Society of Nuclear Medicine and Molecular Imaging’s 2013 Annual Meeting.
“Using FDG PET we can easily detect changes that occur in the heart at the microscopic level — much sooner than when changes become evident in angiography, at the macroscopic level,” said Arun Sasikumar, M.D., MBBS, lead researcher from the department of nuclear medicine at the Post Graduate Institute of Medical Education and Research (PGIMER) based in Chandigarh, India. “By detecting the detrimental changes in the heart at an early stage, physicians can prescribe medications that can halt disease progression, thus preventing a devastating cardiac event such as heart attack or sudden cardiac death.”
There are several ways to detect CAD, including the use of angiography, which utilizes X-ray energy and contrast dye flushed through major arteries to reveal structural detail about the state of blood vessels, including instances of narrowing and reduced blood flow that develop from plaque build-up and scarring associated with atherosclerosis. Another major method is stress myocardial perfusion imaging (MPI), a molecular imaging technique that provides vital information about heart muscle viability. MPI stress tests tell clinicians about blood flow and aspects of heart function at different levels of stress by bringing patients up to a targeted percentage of their maximum heart rate using either exercise stress or pharmaceutical stress, which provokes effects on the heart similar to those of exercise. A third method is the use of the agent F-18 fluorodeoxyglucose (FDG), which is detected by PET. Injected FDG disperses through the heart and acts like glucose as an energy source for cardiac cells. This method clearly demonstrates actual heart function and blood flow before major narrowing, or stenosis, and reduced blood flow, or ischemia, are indicated on conventional angiographies.
For this study, researchers compared angiography with two molecular imaging methods, exercise stress MPI with the agent Tc-99m tetrofosmin and exercise stress F-18 FDG cardiac PET imaging, to see which performed best for CAD detection. A total of 45 patients with a mean age of 51 participated in the study. Each had some suspected CAD upon evaluation, but no history of heart attack. Every subject was prescribed dietary restrictions and underwent exercise stress tests on separate days, followed by an angiogram within a month.
Angiography was performed as a baseline imaging protocol for comparison between MPI and FDG PET. Abnormal angiograms were found for 27 patients, with at least one of their arteries narrowed by more than 50 percent. Disease staging was organized into three categories of single-, double- or triple-vessel disease.
Results of the comparison between angiograms and two molecular stress tests indicated that 17 patients had single-vessel disease and were better imaged by FDG PET imaging than by MPI. A total of five patients had double-vessel disease, and another five were found to have triple-vessel disease. Results comparing MPI and FDG PET for multivessel disease detection were similar, but the latter was far superior for single-vessel disease. FDG PET was shown to have 96 percent sensitivity while detecting less than 50 percent stenosis of coronary arteries, compared to about 56 percent sensitivity with MPI. Specificity, the method’s accuracy when detecting CAD at this level, was measured at 76 percent for FDG PET and 62 percent for MPI, proving that FDG PET catches earlier stages of disease.
“This research is extremely important because it opens up the possibility of using nuclear medicine in preventive cardiology,” said Sasikumar. “FDG PET imaging can detect ischemia at a very early stage, even before significant symptoms appear. This molecular imaging technique could potentially be used for initial CAD screening to help doctors better determine a patient’s cardiac risk and manage the care of these patients, who would otherwise be considered to have normal cardiovascular function.
Cardiac events occur about every 34 seconds in the United States, and every minute someone is estimated to die from heart disease, according to the American Heart Association. The Centers for Disease Control estimates that 600,000 people die annually of heart disease in the United States — one out of every four deaths. Coronary heart disease is considered to be the single most prevalent form of cardiovascular disease, killing more than 385,000 Americans every year.
For more information: www.snmmi.org


 November 17, 2025
November 17, 2025 







![Phase III clinical trial of [18F]flurpiridaz PET diagnostic radiopharmaceutical meets co-primary endpoints for detecting Coronary Artery Disease (CAD)](/sites/default/files/styles/content_feed_medium/public/Screen%20Shot%202022-09-13%20at%203.30.13%20PM.png?itok=2w6OoNd6)
