Getty Images
May 20, 2022 — Results from a real-world study investigating safety and effectiveness of clopidogrel versus aspirin monotherapy beyond 12 months after PCI in high-risk patients during the chronic maintenance period. This study found that clopidogrel monotherapy was associated with reduced risk of net adverse clinical events (NACE; all-cause death, MI, stent thrombosis, stroke, or BARC type 2, 3, or 5 bleeding) and MACCE (death, MI, stent thrombosis, stroke), and a numerical decrease in major or clinically relevant nonmajor bleeding (BARC type 2, 3, or 5 bleeding), compared with aspirin monotherapy. The findings were presented today as late-breaking clinical research at the Society for Cardiovascular Angiography & Interventions (SCAI) 2022 Scientific Sessions.
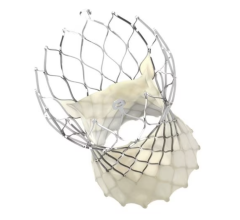
P2Y12 inhibitor monotherapy reduces bleeding risk without increasing the risk of ischemic events compared with dual antiplatelet therapy (DAPT), especially in the first 12 months following percutaneous coronary intervention (PCI). Recent research showed that among patients who were event free for six to 18 months post-PCI and successfully received the intended duration of DAPT, clopidogrel monotherapy was superior compared with aspirin monotherapy in terms of NACE. However, optimal antiplatelet monotherapy during the chronic maintenance period beyond 12 months after PCI with drug-eluting stents in high-risk patients in real-world settings is previously unknown.
In total, 8,377 consecutive patients at high risk for both bleeding and thrombosis were identified from the prospective Fuwai PCI Registry if they satisfied one clinical and one angiographic criterion. Patients who received antiplatelet (aspirin or clopidogrel) monotherapy longer than 12 months and were free from ischemic and bleeding events at 12-month post-PCI without extended duration of DAPT were included. The primary endpoint was net adverse clinical events (NACE) from 12 to 30 months. The key secondary endpoints were major adverse cardiac or cerebral events (MACCE) and major or clinically relevant nonmajor bleeding (BARC type 2, 3 or 5).
“These findings show for the first time clopidogrel monotherapy is associated with reduced risk of long-term NACE and MACCE,” said Hao-Yu Wang, Cardiometabolic Medicine Center, Coronary Heart Disease Center, Department of Cardiology, Fuwai Hospital, State Key Laboratory of Cardiovascular Disease, National Center for Cardiovascular Diseases, Chinese Academy of Medical Sciences and Peking Union Medical College, Beijing, China. “Our results may have important practical implications for determining the optimal treatment for patients requiring a single antiplatelet drug, either aspirin or clopidogrel, for secondary prevention of ischemic events in high-risk PCI population.”
Of 7,392 high-risk patients that were event-free after the first year and adherent to DAPT, 5,664 patients who received antiplatelet monotherapy (clopidogrel monotherapy: n=1,974 and aspirin monotherapy: n=3690) were included in the present analysis. Researchers found that between 12 and 30 months, the net adverse clinical events were lower with clopidogrel monotherapy compared to aspirin monotherapy (Kaplan-Meier estimate: 2.5% vs. 5.0%; adjusted HR:0.566, 95% CI: 0.403-0.795). Clopidogrel monotherapy was associated with lower risk for MACCE (Kaplan-Meier estimate: 1.0% vs. 3.1%, log-rank p = 0.001 ), as well as lower incidence rates of all-cause death, MI, and stroke. The difference in risk between the groups was statistically similar for major or clinically relevant nonmajor bleeding (Kaplan-Meier estimate: 1.5% vs. 2.1%, log-rank p = 0.199).
Researchers recommended that their findings should be further investigated through a randomized clinical trial.
For more information: www.scai.org
Find more SCAI22 coverage here
Related Clopidogrel Monotherapy content:
One-month Clopidogrel Monotherapy After PCI Not Supported in STOPDAPT-2 ACS Trial
Stopping DAPT After One Month Improved Outcomes in Stent Patients
Ticagrelor Not Superior to Clopidogrel in Reducing Heart Attacks During PCI


 May 05, 2025
May 05, 2025