A Chinese registry study found there are higher event rates in patients with shorter dual-antiplatelet therapy (DAPT) after PCI procedures. There has been a lot of movement toward using shorter duration DAPT with newer generation drug-eluting stent technologies, but this study reinforces the need longer DAPT in many patients. The findings were presented as a late-breaking trial at SCAI 2021 today.
April 28, 2021 — An analysis of the prospective Chinese Fuwai PCI Registry, confirms long-term, dual-antiplatelet therapy (DAPT) is an optimal treatment option for acute coronary syndrome patients (ACS) following a percutaneous coronary intervention (PCI). The study shows long-term DAPT reduces ischemic events without increasing bleeding or other complications as compared to short-term DAPT treatments.
The study. Establishing the Optimal Duration of DAPT After PCI in High-Risk TWILIGHT-like patients with Acute Coronary Syndrome, was presented today as late-breaking clinical research at the Society for Cardiovascular Angiography and Interventions (SCAI) 2021 Scientific Sessions.
Following ACS, patients have a high risk of ischemic events, which impacts chances of survival.[1,2] Patients are predisposed for blood clots within an artery for years after an ischemic event,[3,4,5] suggesting that the pathobiology of recurrent events post-ACS differs from that of stable coronary artery disease (CAD) patients who have not offered a previous ischemic event. Therefore, ACS patients may be more likely to benefit from long-term secondary prevention strategy, like extended duration DAPT.
DAPT with aspirin and a P2Y12 inhibitor is the cornerstone of management after an ACS.[6] Current practice guidelines recommend treatment of ACS patients include more aggressive risk factor modification and prolonged antiplatelet therapy, as well as DAPT for a minimum of 12 months following an ACS, regardless of whether or not PCI is performed.[7,8] In addition to protecting against stent thrombosis in the culprit lesion, an important objective of long-term DAPT in patients with ACS is the prevention of future coronary ischemic events from nonculprit lesions, as demonstrated in earlier trials.[9,10,11,12] With the improvement of stent device technology, studies evaluating the safety and efficacy of shortening DAPT to less than 12-months in patients with ACS undergoing PCI reported conflicting results.[13,14,15]
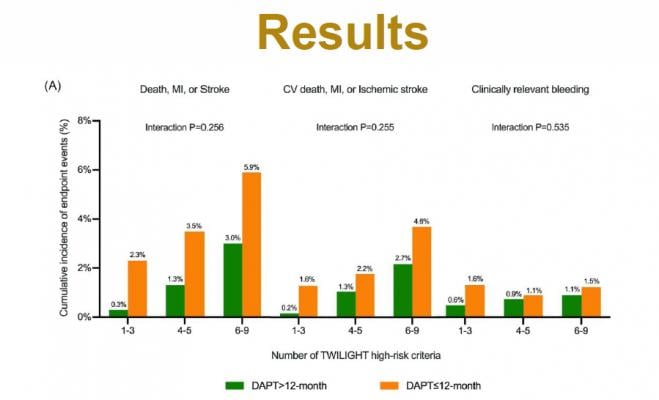
The study included 4,875 high-risk “TWILIGHT-like” patients undergoing PCI. The high-risk patients were defined by at least one clinical and one angiographic feature based on TWILIGHT trial selection criteria, with ACS who were event free at 12 months after PCI from the Fuwai PCI Registry. The primary outcome was the composite of all-cause death, MI or stroke at 30 months while the Bleeding Academic Research Consortium (BARC) type 2,3 or 5 bleeding was key secondary outcome. Results showed that slightly more than two-third of ACS patients remained on DAPT beyond 12 months after PCI. Extended DAPT compared with shorter DAPT reduced the composite outcome of all-cause death, MI or stroke by 63%. BARC type 2, 3, or 5 bleeding rates did not differ significantly in patients treated with DAPT longer than 12-months versus those treated with DAPT less than 12-months. The effect of long-term DAPT on primary and key secondary outcome across the proportion of ACS patients with 1-3, 4-5, or 6-9 risk factors showed a consistent manner.
“Our findings suggested that prolonged DAPT in ACS patients who present with a particularly higher risk for thrombotic complications without excessive risk.” said Haoyu Wang, M.D., Fuwai Hospital, National Center for Cardiovascular Diseases, Chinese Academy of Medical Sciences and Peking Union Medical College, China. “Not only did we see long-term DAPT was associated with a lower risk of a major cardiovascular event without an increase in bleeding events, but it it could be considered an effective strategy to balance the risk for bleeding and ischemia in high-risk patients with ACS. Our results reinforce prolonged DAPT in patients with acute coronary syndrome without excessive risk of bleeding should remain the standard of care.”
Authors call for further analysis on high bleeding risk and ischemia patients and work to publish in additional publications across Asia.
References:


 August 28, 2023
August 28, 2023 









