Getty Images
November 20, 2023 — In the U.S., nearly 10,000 children and adolescents have developed a condition called multisystem inflammatory syndrome, or MIS-C, following COVID-19 infection. MIS-C is a serious, potentially life-threatening illness that results in inflammation, with the cardiovascular system frequently affected. During the acute phase of the disease, some patients experience acute cardiac injury, while others do not. Investigators at Children’s Hospital Los Angeles analyzed results of follow-up cardiac studies for all children who had been hospitalized at CHLA for MIS-C. They found that many patients with MIS-C had abnormal findings on at least one cardiac study at their 6-month follow-up. Also, the proportion of abnormal findings was not significantly different between patients who experienced cardiac injury during their hospitalization compared with patients who did not have overt cardiac complications during their hospitalization.
Results of the study have been published in the journal Pediatrics.
“We wanted to find out if there were any lingering cardiac effects in children treated for MIS-C, given that some of them were so ill they needed to be admitted to the intensive care unit, but then went on to make what looked like a complete clinical recovery,” says Jackie Szmuszkovicz, MD, a pediatric cardiologist at CHLA, Medical Director of the hospital’s Kawasaki Disease Program and co-senior author on the study.
Although other centers have focused their follow-up studies on patients who had evidence of cardiac complications during the acute phase of the disease, investigators at CHLA opted to include all patients who returned for follow-up—whether or not they had experienced cardiac injury during hospitalization.
“At Children’s Hospital Los Angeles, we care for probably one of the largest populations of MIS-C patients in the country,” says Andrew Cheng, MD, a pediatric cardiologist at CHLA and co-senior author on the study. “We felt like we needed to really find out how these kids were doing before they got an ‘all clear.’”
Sixty-nine patients returned to CHLA for at least one follow-up cardiac evaluation and were included in the analysis. Overall, muscle contractions of the heart appeared normal. Cardiac health was assessed further using three measures to detect more subtle changes:
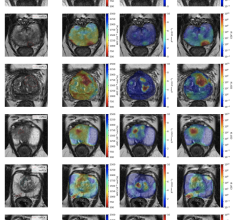
- Cardiac MRI—to provide information about the health of the heart muscle, such as the presence of inflammation and scar tissue, and how well it was functioning
- Ambulatory heart rhythm monitoring—to check for arrhythmias by continuous monitoring
- Cardiopulmonary exercise stress testing—to determine the health of the heart and lungs and the child’s ability to exercise to their maximum potential
The most common finding was an abnormal MRI measurement of the health of the heart muscle. The investigators suggest further follow-up is needed to determine if this is from inflammation or if there could be permanent damage, like scarring. Nine percent of patients had a documented arrhythmia. This change in the normal heart rhythm could be transient or may be a result of damage to the heart that could predispose the child to having an abnormal heart rhythm and the health consequences of this condition later in life. Using exercise stress testing, the investigators saw a number of children who had lower than expected exercise capacity. However, this finding was complicated by the fact that children became sedentary during the pandemic, which may have also impacted their exercise capacity.
Overall, the testing showed that subclinical cardiac effects were seen in many patients who had been treated for MIS-C.
“We were surprised to see that many patients had some sign of cardiac pathology, so we recommend that all patients who had MIS-C receive a cardiac follow-up evaluation,” says Dr. Szmuszkovicz. “The extent of cardiac abnormalities varied, with some changes being quite subtle. Whether these changes are transient or permanent is still unknown. However, if the damage is permanent, these kids are potentially at lifelong risk of early heart disease. It is important to know now so that steps can be taken to help mitigate that risk.”
Other contributors to the study, all from Children’s Hospital Los Angeles, include: first author, Dayna Zimmerman, MD; Andrew Souza, DO; Jennifer A. Su, MD; Jodie Votava-Smith, MD; Sharon Wagner-Lees, RN; and Kelli Kaneta, MD.
For more information: www.chla.org
Related Content on MIS-C:
Kawasaki-like Inflammatory Disease Affects Children With COVID-19
Case Study Describes One of the First U.S. Cases of MIS-C
NIH-funded Project Wants to Identify Children at Risk for MIS-C From COVID-19
New Study Looks at Post-COVID-19 Emerging Disease in Children
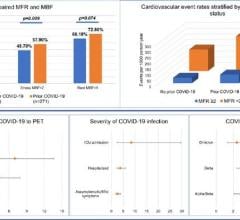
The Cardiovascular Impact of COVID-19
VIDEO: Example of a Multisystem Inflammatory Syndrome in Children (MIS-C) Pediatric Echocardiogram
NIH-funded Project Wants to Identify Children at Risk for MIS-C From COVID-19
Related COVID-19 in Children Content:
Kawasaki-like Inflammatory Disease Affects Children With COVID-19
How COVID-19 Affects the Brain in Neuroimaging
CT Findings of Coronavirus in Children Often Negative
Related COVID-19/Heart Damage Content:
Getting to the Heart of COVID-19 Vaccination and its Cardiovascular Risks
COVID-19 Surges Linked to Spike in Heart Attacks
COVID-19 Fallout May Lead to More Cancer Deaths
Kawasaki-like Inflammatory Disease Affects Children With COVID-19
FDA Adds Myocarditis Warning to COVID mRNA Vaccine Clinician Fact Sheets
CMS Now Requires COVID-19 Vaccinations for Healthcare Workers by January 4
Cardiac MRI of Myocarditis After COVID-19 Vaccination in Adolescents
Small Number of Patients Have Myocarditis-like Illness After COVID-19 Vaccination
Overview of Myocarditis Cases Caused by the COVID-19 Vaccine
Case Study Describes One of the First U.S. Cases of MIS-C
NIH-funded Project Wants to Identify Children at Risk for MIS-C From COVID-19

 March 20, 2024
March 20, 2024