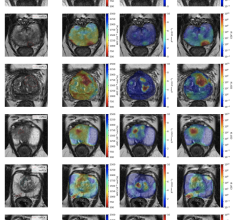
54-year-old patient with COVID-19 who underwent full angiographic reperfusion (extended thrombolysis in cerebral ischemia score = 3) after acute ischemic stroke. Top: Automated readout summary of CT perfusion data at presentation shows large mismatch volume (54 mL). Bottom: Follow-up MR image shows progression in infarction growth, with final infarction volume of approximately 72 cm3 (600% increase from CT perfusion imaging estimate of 9 mL shown in A).
May 18, 2023 — According to an accepted manuscript published in ARRS’ own American Journal of Roentgenology (AJR), SARS-CoV-2 infection may promote continued infarction progression, despite angiographic reperfusion, in vaccine-naïve patients with large-vessel occlusion acute ischemic stroke (AIS).
“The findings carry potential implications for prognostication, treatment selection, and surveillance for infarction growth among revascularized patients in future waves of infection by novel viral strains,” wrote first author Seena Dehkharghani, MD, director of stroke and cerebrovascular imaging at New York University Langone Medical Center.
This AJR accepted manuscript compared 100 consecutively presenting patients with COVID-19 and AIS between March 2020 and April 2021 with a contemporaneous cohort of 282 patients with AIS who did not have COVID-19. Reperfusion classes were dichotomized into positive (extended thrombolysis in cerebral ischemia [eTICI] score = 2c–3) and negative (eTICI score < 2c) groups. All patients underwent endovascular therapy following initial CT perfusion imaging (CTP) to document infarction core and total hypoperfusion volumes.
Ultimately, in this case-control study of vaccine-naïve patients with and without COVID-19 with infarct growth after endovascular reperfusion during acute ischemic stroke, COVID-19 was a significant predictor for absolute infarct growth of 15 cm3 or more (OR, 5.1 [95% CI, 1.0–25.95]; p = .05).
“These findings support the potentially aggressive clinical course of cerebrovascular events in patients with COVID-19, suggesting greater infarction growth and ongoing consumption of at-risk tissues, even following angiographic reperfusion,” Dehkharghani et al. added.
For more information: www.arrs.org

 March 20, 2024
March 20, 2024