New study finds children treated for MIS-C had normal heart function within three months after their first symptoms.
January 19, 2022 — Heart function recovery returned within three months in children who developed COVID-19 related multi-system inflammatory syndrome (MIS-C), according to new research published today in the Journal of the American Heart Association, an open access, peer-reviewed journal of the American Heart Association (AHA).[1]
MIS-C is a new illness identified during the COVID-19 pandemic that affects children about four to six weeks after exposure to COVID-19. The new condition has some overlapping symptoms with Kawasaki disease, however, MIS-C is associated with more profound inflammation. MIS-C can cause inflammation in different parts of the body, including the heart, lungs, kidneys and gastrointestinal organs. About 80%-85% of MIS-C cases across the U.S. and Europe have involved the heart’s left ventricle.
This study details the cardiovascular complications or damage found during a three-month follow-up period to assess the short-term impact of MIS-C. It also employs newer cardiac measurements, known as “strains,” to assess heart function related to MIS-C. Strain testing is a more sensitive tool that can detect whether an area of the heart is deformed or if there are any subtle changes in heart function during cardiac contraction and relaxation.
“There is limited data at this time about how frequently and how long we should monitor heart function during the recovery state of MIS-C after the child leaves the hospital,” said the study’s senior author Anirban Banerjee, M.D., a professor of clinical pediatrics at the University of Pennsylvania Perelman School of Medicine and an attending cardiologist with the Cardiac Center at the Children’s Hospital of Philadelphia, both in Philadelphia.
“Given that MIS-C was identified as a result of the COVID-19 pandemic, treatment protocols have not yet been standardized and follow-up care varies greatly, which may lead to confusion and anxiety among families of patients and their care team. Our research team hoped to provide some guidance and reduce the ambiguity on optimal care approaches, especially as it relates to sports participation,” Banerjee added.
Researchers retroactively reviewed data on 60 children hospitalized with MIS-C due to COVID-19 exposure who were treated at two Philadelphia hospitals between April 2020 and January 2021. None of the children were initially diagnosed with COVID-19 before the onset of MIS-C symptoms. This group of children were 60% male, with an average age of 10 years. About 48% were Black children, 27% were white children, 15% were Hispanic children, 4% were Asian children and the race/ethnicity of 23% of the children was unknown. The participants were treated with intravenous immunoglobulin and/or systemic steroids. Researchers reviewed echocardiographic and clinical data from medical records, including demographic factors, testing, treatment and hospital outcomes.
Data on another 60 children who had structurally normal hearts and did not have MIS-C or COVID-19 exposure served as control subjects. Their average age was 11.5 years, and 55% were male; 62% white children, 27% Black children, 7% Hispanic children, 3% Asian and 8% unknown. The control participants were divided into two groups: 60% had echocardiograms on file that were done prior to the COVID-19 pandemic, and 40% had echocardiograms under rigid COVID-19 protocols after October 2020.
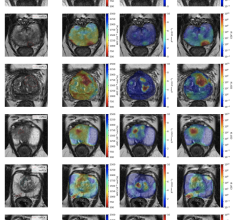
For the children with MIS-C, researchers analyzed images of the heart taken at the initial hospitalization (acute phase) and examined additional imaging for a portion of the children who also had scans up to three additional times – one week after the first scan (subacute phase); at the one-month follow-up; and at a three or four-month follow-up. The children were screened using conventional echocardiography, speckle tracking echocardiography – an imaging technique that analyzes the motion of the heart tissue - and cardiac magnetic resonance imaging (MRI) for images of the heart.
Key Findings of News MIS-C Study
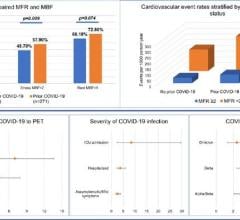
Based on echocardiogram imaging, systolic and diastolic function in the left ventricle and systolic function in the right ventricle improved quickly within the first week, followed by continued improvement and complete normalization by three months.
81% of patients lost some contractile function in the left ventricle during the acute phase of illness, yet, by months three and four, contraction function had returned to normal.
MIS-C did not cause lasting coronary artery abnormalities. During the initial hospitalization, 7% of patients had evidence of some heart malfunction, however, all scans were normal by the three-month follow-up.
Using strain parameters to measure cardiac function, the results suggest that there is no subclinical cardiac dysfunction after three months.
“Recovery among these children was excellent,” Banerjee said. “These results have important implications for our health care teams managing care for children with MIS-C. Our findings may also provide guidance for a gradual return to playing sports after cardiac clearance three to four months later. Tests needed for clearance include electrocardiogram and echocardiogram. We also recommend cardiac MRI for children who have highly abnormal baseline cardiac MRI during the acute stage or show evidence of continued severe left ventricle dysfunction.”
The study researchers note there are still important gaps in existing knowledge about MIS-C, since COVID-19 and MIS-C are both new illnesses. The most important question yet to answer is how these children are faring one to two years after their initial hospitalization.
There are important limitations to note. The study was retrospective for clinical purposes and was not standardized for research. In addition, follow-up data was missing for some patients who dropped out of the study during follow-up stages. Banerjee explained that because both COVID-19 and MIS-C were newly discovered diseases, the timing of follow-up echocardiograms was somewhat arbitrary and driven by preference of different clinicians, rather than standard research protocol.
“The strength of the study is that researchers performed a detailed, serial assessment of cardiac function over the initial three to four months of illness,” according to AHA volunteer expert Kevin G. Friedman, M.D., a member of the American Heart Association’s Young Hearts Council and the AHA’s Rheumatic Fever, Endocarditis and Kawasaki Disease Committee, an attending physician in pediatric cardiology at Boston Children’s Hospital and associate professor of pediatrics at Harvard Medical School, both in Boston.
“This study provides additional evidence that myocardial involvement is transient and may not lead to long-term abnormalities in left ventricular diastolic or systolic function,” Friedman said. “Although cardiac involvement in the acute stage of illness is common, it is reassuring that all patients recovered normal cardiac function within about one week. This data tells us that, fortunately, lasting heart injury is very uncommon in MIS-C. Even in those patients with significant cardiac abnormalities in the acute phase of illness, these changes resolved by 3-4 months.”
Co-authors are Daisuke Matsubara, M.D., Ph.D.; Joyce Chang, M.D., M.S.C.E.; Hunter L. Kauffman, B.S.; Yan Wang, R.D.C.S.; Sumekala Nadaraj, M.D.; Chandni Patel, M.D.; Stephen M. Paridon, M.D.; Mark A. Fogel, M.D.; and Michael D. Quartermain, M.D.
For more information: heart.org
Find additional CDC statistics on U.S. MIS-C cases
Related Content on MIS-C:
Kawasaki-like Inflammatory Disease Affects Children With COVID-19
VIDEO: Overview of Multisystem Inflammatory Syndrome in Children (MIS-C) in COVID-19 Exposed Children — Interview with Deepika Thacker, M.D.
Case Study Describes One of the First U.S. Cases of MIS-C
Study Provides MIS-C Treatment Guidance To Avoid Cardiovascular Dysfunction
NIH-funded Project Wants to Identify Children at Risk for MIS-C From COVID-19
New Study Looks at Post-COVID-19 Emerging Disease in Children
The Cardiovascular Impact of COVID-19
VIDEO: Example of a Multisystem Inflammatory Syndrome in Children (MIS-C) Pediatric Echocardiogram
NIH-funded Project Wants to Identify Children at Risk for MIS-C From COVID-19
Reference:

 March 20, 2024
March 20, 2024