December 16, 2011 – St. Jude Medical began a voluntary recall Nov. 28 for its Riata and Riata ST Silicone Defibrillation Leads, which the U.S. Food and Drug Administration (FDA) has now classified as a Class I recall. An estimated 79,000 Riata and Riata ST family of silicone leads remain active in patients in the United States, although the company stopped selling the leads in December 2010.
The FDA said the silicone insulation covering these defibrillation leads is at risk of premature abrasion. When abrasion occurs, the conductors inside the leads can come out (externalized) of the insulation. Leads with externalized conductors may develop electrical dysfunction and not work as intended. In the event the device does not work as intended, should a life-threatening heart rhythm occur, pacing or defibrillation therapy may not be delivered as intended. This may result in serious adverse events, including death.
Reports to St. Jude Medical associated with extraction of a Riata lead with externalized conductors include two patient deaths and one serious injury (effusion requiring thoracotomy). In addition, one patient death and one serious injury in patients with externalized conductors were reported, but were determined not to be due to the presence of externalized conductors.
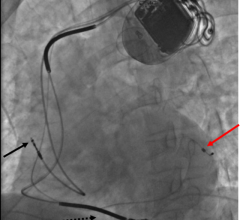
Communicated in a physician advisory letter Nov. 28, 2011, the company said the clinical implications of externalized conductors in a defibrillation lead without electrical anomalies are not fully known or understood at this time. Externalized conductors can present as only a visual observation on X-ray or fluoroscopy without any associated clinical or device-related observations. If the electrical integrity of a lead were to be compromised, failure to deliver appropriate therapy, or the delivery of inappropriate therapy, could potentially occur, and could lead to a serious adverse event or death.
Reports to St. Jude Medical associated with extraction of a Riata lead with externalized conductors include two patient deaths and one serious injury (effusion requiring thoracotomy). In addition, one patient death and one serious injury in patients with externalized conductors were reported, but were determined not to be due to the presence of externalized conductors.
The FDA’s classification updates the recommendations provided in physician advisory letter, which is available on the company’s website, www.sjmprofessional.com.
The affected model numbers are the Riata (8 French) Silicone Endocardial Defibrillation Leads (Models 1560, 1561, 1562, 1570, 1571, 1572, 1580, 1581, 1582, 1590, 1591, and 1592), and the Riata ST (7 French) Silicone Endocardial Defibrillation Leads (Models 7000, 7001, 7002, 7010, 7011, 7040, 7041, and 7042).
St. Jude Medical reiterates that all leads with an externalized conductor, with or without an associated electrical abnormality, be reported to the company’s Technical Services Department at 800.722.3774. The company strongly encourages that any experience with screening of Riata leads for externalized conductors be shared with the company, including information regarding a lead or leads in which externalized conductors are not present. If a lead has been removed from the patient, St. Jude Medical requests that it be returned to the company, at company expense, for failure analysis to further understand this particular failure mechanism. All reports and returns received by St. Jude Medical of Riata leads exhibiting externalized conductors, irrespective of whether there is an associated electrical abnormality, are reported to FDA as a medical device report (MDR). Any adverse reactions experienced with the use of this product, and/or quality problems also should be reported to the FDA’s MedWatch Program by phone at 800.FDA.1088, or on the MedWatch website at www.fda.gov/medwatch.
St. Jude Medical acknowledges that the clinical implications of leads with electrically intact externalized conductors are not fully known at this time. Consequently, more data are required in order to assess if specific patient subgroups with electrically intact externalized conductors are at greater risk or should be managed differently. Patients who require frequent defibrillation or who are pacemaker dependent may be considered to be at greater risk. It is recognized that physicians may choose to individualize the approach to management of electrically intact externalized conductors based on individual patient characteristics. The potential risks associated with externalized conductors as well as the potential risks and benefits of management options should be considered and discussed with patients.
“At this time, no blanket statement can be made about clinical recommendations. Until more data are collected, physicians should follow standard practice of care to manage their patients with Riata silicone leads,” said Anne Curtis, M.D., professor and chair of medicine at the University at Buffalo, former Heart Rhythm Society (HRS) president and a member of St. Jude Medical’s Medical Advisory Board (MAB). Also, over the next several weeks, there are two public meetings scheduled to discuss Riata and associated clinical recommendations: A Riata Leads Issue Webinar sponsored by the Heart Rhythm Society on Dec. 21, 2011 and a Riata ICD Lead Summit sponsored by the Minneapolis Heart Institute Foundation on Jan. 20, 2012. Any additional consensus opinion developed from these meetings, including any additional screening efforts, will be addressed by St. Jude Medical and, if appropriate, will be communicated to the physician community.
The company and its independent MAB have recommended the following related to patient monitoring:
· For leads that do not exhibit externalized conductors, continue to monitor the patient’s implanted system at regularly scheduled visit intervals every three to six months as per Heart Rhythm Society (HRS)/European Heart Rhythm Association (EHRA) consensus with particular attention to diagnostic information related to defibrillation lead performance.
· For leads that exhibit externalized conductors with no electrical abnormality, continue to monitor lead and system performance as per HRS/EHRA guidelines. The value of screening x-ray or fluoroscopy for patients with leads that exhibit no electrical abnormalities is unknown at this time and therefore, the risk of increased radiation exposure for monitoring should be weighed against using remote monitoring and in-clinic follow-up for detection of electrical anomalies. Prophylactic explant or replacement of a lead without electrical dysfunction is not recommended.
· For leads that exhibit externalized conductors with an associated electrical abnormality, management of the patient may include x-ray, fluoroscopy (cine), or additional testing including provocative methods such as shoulder and arm movements and deep respiration while looking at the surface ECG and intracardiac electrograms.[1] Consideration should be given to prophylactically replacing leads with observed electrical abnormalities. If the leads are replaced, the risks and benefits of removing the old leads, or leaving them in place, should be carefully considered.
· Currently there is no expert consensus regarding whether patients undergoing pulse generator replacement should undergo fluoroscopy or lead replacement if an externalized conductor without electrical anomalies is present. This is, in part, because the risk versus benefit of replacing a lead in such a patient may vary from patient to patient and center to center. Consideration of fluoroscopy and lead replacement at time of pulse generator replacement should be individualized based on specific patient conditions and circumstances.
St. Jude Medical strongly encourages that whenever possible, remote monitoring and patient alerts be used to detect as early as possible any electrical changes that may be associated with externalized conductors. Changes in impedance from three high voltage lead vectors (RVC to Can, SVC to Can, and RVC to SVC), as well as pacing and sensing electrodes, can be detected by St. Jude Medical ICDs and provided to the clinician during the in-clinic device evaluation and may also be provided by means of remote monitoring (Housecall+, Merlin@Home, and Merlin.net). Data are displayed graphically to enable physicians to trend changes in impedance over time.
Customized DirectAlerts notifications allow physicians to monitor patient status between follow-ups. The noise reversion feature is designed to protect against non-physiologic high-rate event detection to avoid inappropriate shocks. Standard reprogramming such as turning on the EGM for Noise Reversion or ensuring that the ventricular rate EGMs are set to detection should also be considered. A patient may also become aware of electrical abnormalities even earlier when their device has a patient vibratory alert. Patients who receive a patient vibratory alert should contact their clinician.
In order to improve the understanding of this particular failure mechanism, St. Jude Medical has initiated a prospective study to evaluate the incidence rate and the long term performance of leads found to exhibit externalized conductors without an associated electrical abnormality, including an evaluation of any potential long term degradation of the ETFE insulation that is exposed outside of the silicone insulation. Enrollment has begun and is expected to continue to follow patients for up to two years. As information is gathered during this study, St. Jude Medical will update the physician community and, as appropriate, provide any specific updated recommendations for physicians to manage their patients.
For more information: www.sjm.com
Reference:
- Epstein, A.E. “Troubleshooting of Implantable Cardioverter-Defibrillators.” Clinical Cardiac Pacing, Defibrillation, and Resynchronization Therapy, 3rd ed., Eds. Ellenbogen, K.A., Kay G.N., Lau, C-P., Wilkoff, B.L., Philadelphia: Elsevier, 2007, pp. 1063-1086.


 January 13, 2026
January 13, 2026