
November 14, 2011 – Boston Scientific welcomed positive outcomes from the COBRA clinical trial, which evaluated post-dilation of nitinol stents using CryoPlasty therapy with the PolarCath peripheral dilatation system compared to stenting with conventional balloon angioplasty in patients with diabetes presenting with blockages of the superficial femoral artery (SFA). The trial was funded through an unrestricted grant from Boston Scientific.
Results from the prospective, randomized, multi-center trial demonstrated a significant 47 percent relative reduction in binary restenosis rates for patients treated with nitinol self-expanding stents using post-dilation with the PolarCath System. The analysis was presented today during a late-breaking clinical trial session by principal investigator Subhash Banerjee, M.D., chief of the division of cardiology at VA North Texas Health Care and associate professor of medicine at the University of Texas Southwestern Medical School in Dallas, at the Cardiovascular Research Foundation's annual Transcatheter Cardiovascular Therapeutics (TCT) scientific symposium in San Francisco.
The COBRA trial enrolled 76 patients with 90 SFA lesions who were randomized to CryoPlasty therapy or conventional balloon angioplasty (CBA) for post-dilation of nitinol stents used to treat SFA blockages. Inclusion criteria included diabetes, severe claudication and SFA lesions requiring stents >5 mm in diameter and >60 mm in length. The primary endpoint is the rate of binary in-segment restenosis determined by duplex ultrasonography.
Follow-up data have been completed on 41 lesions in the CryoPlasty group and 43 lesions in the CBA group. Results at 12 months showed that binary restenosis was significantly lower in the CryoPlasty group (29.3 percent versus 55.8 percent, p=0.01). The secondary endpoint of change in the ankle-brachial index (ABI) from baseline to 12 months showed significant improvement in the CryoPlasty group (0.59+0.21 to 0.77+0.30, p=0.004) compared to the CBA group (0.62+0.19 to 0.65+0.26, p=0.66). ABI is the ratio of blood pressure in the lower legs to blood pressure in the arms, which can indicate the presence of blocked peripheral arteries (a higher number indicates less peripheral blockage). Procedural success was achieved in 100 percent of procedures in the CryoPlasty group.
"High restenosis rates remain a major limitation for peripheral stenting in treating patients with peripheral artery disease, particularly in patients with diabetes mellitus," said Banerjee. "Reducing revascularization rates is critical to improving outcomes, and these trial results show that CryoPlasty therapy can significantly reduce binary restenosis at least to 12 months in the studied patient population."
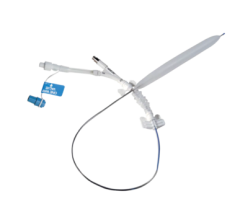
CryoPlasty therapy using the PolarCath peripheral dilatation system is a novel form of balloon angioplasty designed to treat atherosclerotic lesions in the peripheral arteries. This technology uses nitrous oxide in place of standard saline to fill an angioplasty balloon within a blocked artery, cooling the balloon's surface to minus 10 degrees Celsius. As the balloon is inflated, its surface cools and dilates the vascular lesion, potentially helping prevent artery re-blockage.
"CryoPlasty has become a useful treatment option for physicians whose patients are suffering from peripheral artery disease," said Jeff Mirviss, president of Boston Scientific's peripheral interventions business. "The COBRA trial results validate the use of CryoPlasty therapy for post-dilation of peripheral stents to modulate vessel response and potentially lower restenosis rates. Boston Scientific is committed to delivering innovative solutions and is pleased to be the only company to offer the CryoPlasty treatment option as part of our expanding peripheral portfolio."
The PolarCath peripheral dilatation system is approved in the United States for treating blockages in the peripheral vasculature and for post-dilation of self-expanding peripheral vascular stents.
For more information, visit www.cryoplasty.com, www.bostonscentific.com

 June 13, 2024
June 13, 2024 









