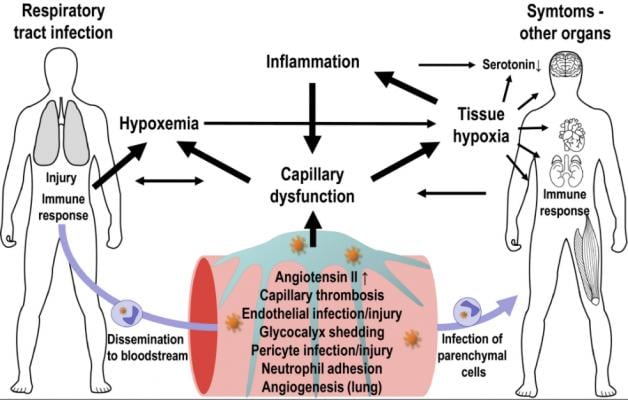
Interactions between capillary function, inflammation, hypoxia, and neurotransmission. The expression of ACE2 and other SARS‐CoV‐2 entry factors on parenchymal cells and observations of infected cells in biopsy material hold important clues to understand COVID‐19‐related organ damage. Find more figures and read the full study.
March 12, 2021 — A new review suggests that blood vessel damage and impaired oxygen delivery related to COVID-19 play a role in mood changes and cognitive difficulties that people with the disease face during illness and recovery. The review was published in Physiological Reports in February.[1] The article offers insights into the reason why some ling-hauler COVID patients have persistent symptoms months after their infections. While the the "brain fog" and cognitive issues are most evident in many of the long-hauler patients, there are concerns over of physiological issues, including the impact on the heart.
COVID-19, the disease caused by the SARS CoV-2 virus, may cause a wide range of symptoms ranging from lack of taste and smell, muscle weakness and fatigue to acute respiratory distress syndrome and multiple organ failure. Changes in blood flow and microscopic clots in the body’s smallest blood vessels can also affect people with the disease. “While most symptoms disappear over the weeks and months following the infection, the extent of long-term COVID-19 [complications] remains unclear,” the authors of the review wrote.
One cluster of symptoms people with COVID-19 have experienced — even after active infection has passed — is cognitive or mood impairment. This may include memory problems, depression, anxiety and the inability to focus or concentrate, which is called “brain fog.” Previous research has found that people with a diagnosis of mild cognitive impairment or Alzheimer’s disease show “widespread cerebral microvascular flow disturbances.” The current review explains that in people with COVID-19, a shortened blood flow transit time in the capillaries limits the amount of oxygen that can be delivered to the lungs and brain.
Low oxygen levels and the increase in inflammatory cytokines — proteins involved in immune system signaling — that occur with COVID-19 can also affect serotonin levels. Serotonin is a neurotransmitter the brain produces to regulate mood. Low levels of serotonin have been linked to anxiety and lowered mood. Oxygen is crucial for the production of serotonin, and research suggests cytokines reduce serotonin levels. “These mechanisms could affect cognitive functions and quality of life for COVID-19 patients,” the reviewers wrote.
Other findings discussed in the review include:
• The recovery of COVID-19 patients may rely on the restoration of normal blood flow through the body’s smallest blood vessels.
• Development of new blood vessels in COVID-19 may form shunts for blood delivery through the lungs and contribute to poor blood oxygenation.
Read the full article, “SARS CoV‐2 related microvascular damage and symptoms during and after COVID‐19: Consequences of capillary transit‐time changes, tissue hypoxia and inflammation,” published in Physiological Reports.
Related COVID-19 Cardiology Content:
The Long-term Cardiovascular Impact of COVID-19
COVID-19 Changes Properties Blood Cells
VIDEO: Antithrombotic Prophylaxis in COVID-19 Patients — Interview with Behnood Bikdeli M.D.
Coronavirus Disease 2019 (COVID-19) and the Heart—Is Heart Failure the Next Chapter?
PHOTO GALLERY: How COVID-19 Appears on Medical Imaging
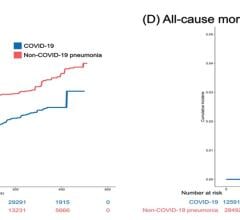
Heart Damage Found in More Than Half of COVID-19 Patients Discharged From Hospitals
Overview of Randomized Trials of Antithrombotic Therapy for COVID-19 Patients
COVID-19 Can Kill Heart Cells and Interfere With Contraction
Reference:

 March 20, 2024
March 20, 2024