While the current positive revolution in percutaneous coronary intervention (PCI) practice has been made possible by the wealth of technological advancements, bringing the necessary tools together in a streamlined workflow has remained a challenge for clinicians. We now appreciate the value of using physiology and intravascular ultrasound (IVUS) to identify the severity and location of ischemia, precisely identify vessel size and characterize plaque morphology, and more accurately plan the intervention. Integration of state-of-the-art technology to act on that information can help clinical teams standardize an elevated level of care, enhancing outcomes while improving efficiencies and reducing costs.
Seeing beyond the angiogram
Angiography has long been accepted as the gold standard for identifying lesions and PCI guidance. Increasingly, interventionalists are augmenting and replacing contrast-based angiography with physiologic and intravascular imaging technologies.1,2 This movement is opening the door to PCI for many patients with reduced renal function and improving overall procedural outcomes. Advancements such as class 1A recommended instantaneous wave-free ratio (iFR), IVUS and co-registration are now considered by many as key elements of a modern precision PCI program. These tools may guide the assessment of “vessels” rather than “lesions” to understand the degree of ischemia and, more importantly, to guide treatment.
Treating more complex cases
Coronary artery disease complexity has been increasing due to comorbidities such as diabetes mellitus and chronic kidney disease (CKD). In addition to disease complexity, the diffuse nature creates a challenge in treating vessels. With advanced technologies such as co-registration, these patients can be treated using ultra-low contrast, with fewer angiograms. An iFR pullback co-registered with fluoroscopy, provides physiological evidence of diffuse versus focal disease and clearly indicates points of greatest pressure drops so that PCI, if indicated, can be planned accordingly. IVUS imaging can be co-registered as well, correlating anatomical morphology data with the physiologically significant segments to enrich the PCI plan. A virtual stent may be drawn on the system, with identification of an estimated delta change of iFR post-stenting, with anatomical proximal and distal landing zones identified on IVUS. This simplifies the intervention with regard to choosing balloon sizes, plaque modifiers and identifying stent size and length.
PCI in chronic kidney disease (CKD) and avoiding acute kidney injury (AKI)
CKD is a growing comorbidity in patients, at times limiting their chance of receiving appropriately indicated and optimal PCI. To manage the risk for these patients, interventionalists can embrace techniques and technologies aimed at reducing contrast use. For example, they can choose to limit themselves to only a few initial angiograms.
Lesion and vessel assessment can be performed in these specific angles obtained with physiology and imaging. Co-registration can be performed without contrast injections in the same angulations.

An encouraging development for these patients is the recent availability of technology designed to reduce the need for additional contrast injections. With dynamic coronary road mapping, initial angiograms can be co-registered in real time with live fluoroscopy to help guide coronary wire introductions. While clinical research on this technology is limited to date, results of the recent DCR4Contrast study will be presented at EuroPCR and Society for Cardiovascular Angiography and Interventions (SCAI) meetings in May 2023 and should shed light on its efficacy in reducing contrast runs or contrast volume.
After each intervention, whether it is atherectomy or balloon angioplasty, IVUS can be used to see the procedure’s effect on plaque and lesion response. Contrast should still be used when needed, as in hemodynamic instability, EKG changes or at the end of the intervention to identify appropriate flow in the vessel.
Standardize workflow to improve clinical and operational performance
Currently cath labs make up one of the least standardized areas of a hospital, and therefore represent an ample opportunity to reduce variability in the delivery of care. While investing in new technology can be costly, the importance of standardization across this area becomes clear when considering the benefits of technologies that work seamlessly together to reduce variability in the delivery of care. If each lab in a facility has the same integrated set of tools, and if those tools are easy to access, it becomes less challenging for clinical teams to provide a consistently high level of care for every PCI patient, no matter which lab they’re using for the procedure.
“Think of a loved one undergoing PCI. Whether or not there is kidney disease, every patient should be treated with the same standard of care, with high-quality, low-contrast PCI to limit exposure to a nephrotoxic agent and provide the best outcome.”—Dr. Karim Al-Azizi |
There are many vendors who offer excellent physiology and imaging tools, but it was important for us to consider the benefit of technologies that integrate to improve workflows and outcomes. Easy access to applications and imaging tools is essential from diagnosis to treatment, so we chose to standardize on the Philips suite of coronary solutions. Philips IntraSight allows clinicians to perform IVUS and physiologic iFR measurements to accurately identify the location of lesions causing ischemia and precisely place and optimize stents. For even greater accuracy, the platform also offers SyncVision, which includes co-registration and tri-registration of both modalities. Because the IntraSight application is fully integrated into the Philips Azurion image-guided therapy platform, our clinicians can access both iFR and IVUS, as well as the Dynamic Coronary Roadmap, from the Azurion tableside touchscreen monitor, saving time and reducing the need to break scrub. While patients benefit from more consistent care and increased use of physiology and intravascular imaging, our hospital gains greater efficiency.
A more complete view for a successful PCI
To its credit, our specialty has, more than others, led the way in evidence-based clinical decision-making. Now it’s time for us to take the next step and further expand our use of physiology, IVUS and co-registration tools to simplify complex interventions, making care more accessible to at-risk populations, speeding routine procedures, and improving lab efficiency. It’s time to see beyond the angiogram to treat PCI patients optimally with confident decision-making at every step.
1 Xiao-Fei Gao, et al, May 2020 online in US Cardiology Review at Intravascular Ultrasound-guided Versus Angiography-guided Percutaneous Coronary Intervention: Evidence from Observational Studies and Randomized Controlled Trials | USC Journal
2 Alexander G Truesdell, et al, Feb. 2023 Published by Elsevier Inc.: Intravascular Imaging During Percutaneous Coronary Intervention: JACC State-of-the-Art Review - PubMed (nih.gov)
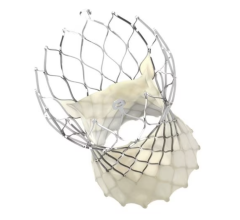
 Karim Al-Azizi, M.D., is a board-certified, interventional cardiologist and structural heart disease specialist at Baylor Scott & White Health – The Heart Hospital, Plano, Texas. In addition, he has completed extensive training in structural heart disease and interventions. He specializes in valvular heart disease, transcatheter valve interventions (e.g., TAVR), left atrial appendage closure, coronary angiography, complex percutaneous coronary interventions (PCI), peripheral vascular disease and interventions. His expertise also includes advanced cardiac imaging technology, including computed tomography (CT), nuclear cardiology and echocardiography.
Karim Al-Azizi, M.D., is a board-certified, interventional cardiologist and structural heart disease specialist at Baylor Scott & White Health – The Heart Hospital, Plano, Texas. In addition, he has completed extensive training in structural heart disease and interventions. He specializes in valvular heart disease, transcatheter valve interventions (e.g., TAVR), left atrial appendage closure, coronary angiography, complex percutaneous coronary interventions (PCI), peripheral vascular disease and interventions. His expertise also includes advanced cardiac imaging technology, including computed tomography (CT), nuclear cardiology and echocardiography.
©2023 Koninklijke Philips N.V. All rights reserved. Approved for external distribution.
D062397-00 042023


 May 05, 2025
May 05, 2025