July 18, 2014 — The Children's Hospital of Philadelphia (CHOP) launched the Fetal Neuroprotection and Neuroplasticity Program. Building on growing evidence of the interaction of heart disease and brain development in the fetus, this program will systematically investigate innovative therapies to protect brain development and to prevent brain injury as early as possible before birth. A joint project of the Hospital's Cardiac Center, the Fetal Heart Program, the Center for Fetal Diagnosis and Treatment, and the Division of Neurology, it is the first-ever comprehensive program dedicated to prenatal neuroprotection.
Unparalleled expertise from many of CHOP's divisions including the Cardiac Center, Center for Fetal Diagnosis and Treatment, Neonatology and Radiology makes this program truly unique. While this program will initially focus on the fetus with congenital heart disease, it will expand in the future to include fetuses with other birth defects, such as congenital diaphragmatic hernia (CDH) andpulmonary hypoplasia.
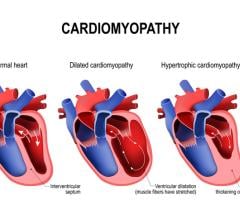
In the United States, approximately one in every 120 newborns is diagnosed with congenital heart disease (CHD), making it the most common birth defect. Many newborns with CHD require either corrective or palliative open-heart surgery. As recently as the 1960s, only 20 percent of newborns with critical CHD survived to adulthood.
"Today, thanks to better diagnostic technologies and methods, including prenatal diagnosis, advances in surgery, and improved postoperative care, early survival is over 90 percent," said J. William Gaynor, M.D., cardiac surgeon and director of the Fetal Neuroprotection and Neuroplasticity Program at The Children's Hospital of Philadelphia. "However, with improved early outcomes has come the sobering recognition that there is an ongoing risk of late mortality as well as significant morbidity for these children. Indeed, neurodevelopmental disability is now recognized as the most common complication of critical CHD — those patients requiring cardiac surgery in infancy — and has the most negative impact on quality of life, academic performance and opportunity for independence as an adult."
Most studies of treatments to prevent brain injury in children with CHD have focused on the intra-operative period and management of cardiopulmonary bypass; however, there is convincing evidence that risk for brain injury begins even before birth. This research, much of it developed at CHOP, shows that in utero brain development is abnormal in fetuses with CHD, leading to delayed maturation, poor growth and white matter injury. These findings suggest that in order to prevent brain injury and improve outcomes, treatment to protect the brain must be initiated before birth.
"Almost half of the children born with CHD have problems in school with math and handwriting, and at least one-third of the population is held back a grade. We know we can make sound diagnoses and the surgical outcomes are excellent, but we're only beginning to learn what proportion of children growing up with CHD will graduate from high school, go to college and obtain a job. We need to improve long-term quality of life in our patients," added Gaynor.
"The lifetime continuum of care for congenital heart disease starts in utero," said N. Scott Adzick, M.D., surgeon-in-chief at The Children's Hospital of Philadelphia. "We now have an opportunity to not only offer the best diagnostic care to the fetus with heart disease, but to also begin to explore ways in which we can optimize long-term outcomes from the neurocognitive perspective. Early identification before birth and early intervention at time of diagnosis offers the best opportunity for optimal results. As a leading center in prenatal care for birth defects, we are committed to discovering the best ways to improve long-term outcomes."
The focus of the new program will be to investigate the factors which cause abnormal brain development in the fetus with a congenital heart defect, and for the first time, to conduct clinical trials of fetal interventions to determine whether novel prenatal treatments can reduce brain injury and improve neurodevelopmental outcomes in newborns with CHD who subsequently undergo cardiac surgery. The first such study will evaluate whether the hormone progesterone, administered prenatally to the mother, has a neuroprotective effect on brain development. "Progesterone is already widely used with few adverse effects in patients," said Mark P. Johnson, M.D., obstetrical director in the Center for Fetal Diagnosis and Treatment at CHOP. "This preliminary trial, comparing a treatment group with controls, will test its effectiveness in children with CHD."
The Children's Hospital of Philadelphia has long been a leader in pediatric cardiac care. More than 30 years ago, CHOP pioneered life-saving early surgeries for children with complex heart defects. Today, most forms of heart disease can be detected prior to birth.
Over the past 15 years, the Fetal Heart Program in conjunction with the Center for Fetal Diagnosis and Treatment at The Children's Hospital of Philadelphia has evaluated thousands of mothers carrying fetuses with heart disease and has provided a unique collaborative approach to the comprehensive care of mother and fetus. A team of dedicated fetal cardiologists, fetal heart sonographers and nurse coordinators offers state-of-the-art care. Both maternal and fetal care are optimized through delivery in the Garbose Family Special Delivery Unit, the world's first birth facility specifically designed for healthy mothers carrying babies with known birth defects. Babies born here will either undergo fetal surgery to treat the birth defect before birth or need immediate specialized care or surgery after birth.
CHOP has a long history in conducting research trials assessing neurodevelopmental outcomes in children with CHD, and showing that fetuses with CHD have abnormal brain development. The NeuroCardiac Care Program at CHOP was the first multidisciplinary program to assess congenital heart disease patients for neurodevelopmental complications, learning disabilities and behavioral concerns, such as being diagnosed with ADHD when children attain school age.
"The Fetal Neuroprotection and Neuroplasticity Program is another innovative initiative in a long series of identifying opportunities to ensure that children with CHD not only survive, but truly thrive, as they grow into adulthood," added Gaynor. "This program allows us to enhance our continuum of care from conception through adulthood."
As heart disease is highly variable, not every family who comes to the Cardiac Center for care will be involved with the Fetal Neuroprotection and Neuroplasticity Program. However, families may still avail themselves of other programs at the Hospital.
CHOP's comprehensive offering of specialized services, including the Fetal Heart Program, the Center for Fetal Diagnosis and Treatment, the Garbose Family Special Delivery Unit and the NeuroCardiac Care Program, provides an unparalleled breadth and depth of medical expertise. Furthermore, if prenatal neuroprotective approaches are proven to benefit patients with CHD, such strategies might be applied to other fetuses at risk for brain injury.
For more information: www.chop.edu


 March 31, 2025
March 31, 2025