May 19, 2011 - Results from a study validating Cheetah Medical's noninvasive NICOM system specifically for use in patients with pulmonary hypertension were presented Wednesday, May 18th, at the 2011 American Thoracic Society Annual Meeting in Denver.
Pulmonary hypertension (PH) is a life threatening condition that affects the heart and lungs. The cause is gradual narrowing of the lung's arteries, which severely impedes blood to flow normally from the heart through the lungs. This means the heart has to work harder than normal to push the blood through the lungs. Over time, the heart weakens and cannot keep up so that blood flow decreases. Eventually, the heart becomes so weak that it can't pump enough blood to meet the demands of the body, even at rest, which leads to the debilitating symptoms of heart failure such as shortness of breath at rest or during minimal activity (for example, climbing two flights of stairs), tiredness, swelling of the legs and stomach, and palpitations (abnormal heartbeats).
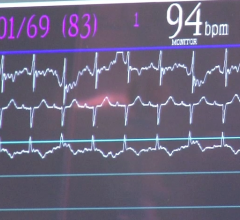
Clinicians have been seeking better ways to monitor disease progression in order to refine treatment. However, traditional methods to assess patients' hemodynamic parameters, and most notably patients' cardiac output (CO), are highly invasive and thus suboptimal for routine serial assessment of PH.
In this study, the Cheetah Medical NICOM (Noninvasive Cardiac Output & Hemodynamic Monitoring System) was used to monitor the hemodynamic performance of 25 pulmonary hypertension patients. University of Chicago researchers compared the results obtained with NICOM to those obtained with two gold-standard methods, which are also invasive: the pulmonary artery catheter, also known as Swan-Ganz catheter, and the Fick method. The NICOM system provided equally accurate and precise measurements to the standard methods, but was completely non-invasive.
Stuart Rich, MD, professor of medicine at the University of Chicago and the study's principal investigator, said, "Survival in patients with pulmonary hypertension is closely linked to their cardiac output. However, because cardiac output measurements have required invasive cardiac catheterization, patients do not have this measured often. With the validation of a simple noninvasive technique to measure cardiac output in these patients, physicians should now be able to evaluate their patients' status frequently, and better judge the efficacy of their treatments."
Researchers hope that these findings will encourage use of CO monitoring not only into routine clinical practice to provide objective means of tracking changes in disease status and response to therapy, but will also pave the way to explore the utility of this technique in clinical trials as an early screening tool for differentiating effective versus non-effective treatments for PH.
For more information: www.cheetah-medical.com


 January 13, 2026
January 13, 2026