Photo credit: Getty Images 2022
November 10, 2022 – Significant findings from the clinical trial, known as “BEST-CLI — Best Endovascular versus Best Surgical Therapy for Patients with Critical Limb Ischemia,” were presented Nov. 7 during the American Heart Association Scientific Sessions 2022, and simultaneously published in the New England Journal of Medicine (NEJM). The study indicates optimal treatment for patients with limb-threatening ischemia.
Investigating two forms of treatment commonly used to restore bloodflow to the leg, researchers sought to identify which treatment approach leads to better outcomes — surgical bypass (Bypass) and endovascular therapy (Endo).
A randomized, multicenter, international clinical trial was led by investigators from Boston Medical Center and Mass General Brigham’s founding members — Brigham and Women’s Hospital (BWH) and Massachusetts General Hospital (MGH). The highly-anticipated trial compared important clinical, patient experience and cost outcomes for the two approaches.
An AHA news release noted the following research highlights:
- A study of more than 1,800 people with severe peripheral artery disease, or PAD, compared the clinical, safety, quality of life and cost outcomes between those who had bypass surgery and those who had angioplasty and stenting to restore blood flow to their feet and legs.
- Researchers determined that for people who are candidates for either procedure and who have a large leg vein that is suitable for bypass surgery, the bypass surgery resulted in fewer repeat procedures and amputations.
Lead Investigators Offer Insights
“Our study provides high-quality clinical evidence to inform the conversations we as clinicians routinely have with our patients when we need to make an important decision about treatment,” said co-principal investigator Alik Farber, MD, MBA, chief of the Division of Vascular and Endovascular Surgery at BMC and professor of Surgery and Radiology at Boston University Chobanian & Avedisian School of Medicine. He added, “Our findings support complementary roles for these two treatment strategies and emphasize the need for pre-procedural planning to assess patients and inform what treatment is selected.”
“We know the best guide for clinicians in caring for their patients is evidence-based decision making,” said Matthew Menard, MD, co-director of the Endovascular Surgery Program at BWH, who was co-principal investigator of the trial. “There’s a large body of evidence from randomized, controlled clinical trials that helps inform strategies for treating or preventing heart attacks and stroke, but up until now, there has been very little data to guide treatment decisions for PAD and CLTI patients. The goal of our work is to try to fill in some of the key missing pieces,” added Menard.
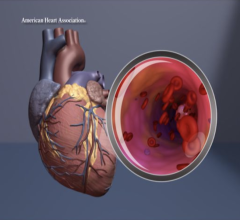
Peripheral Artery Disease (PAD) occurs when the arteries that carry blood away from the heart to the head, arms, legs and feet become narrow due to a build-up of fatty plaque. It affects more than 200 million people worldwide, and its prevalence is increasing because people are living longer, and more people have Type 2 diabetes, a major risk factor for PAD. The artery build-up results in ischemia, or poor blood flow, to the legs and feet. People with severe PAD may develop chronic limb-threatening ischemia (CLTI), which leads to a high risk for limb amputation and causes pain even while at rest, nonhealing wounds or ulcerations, and tissue damage to the foot and leg.
Study Process and Outcomes
BEST-CLI enrolled more than 1,800 patients from sites in the U.S. and abroad. Patients enrolled in the trial were randomized to receive Bypass or Endo in two parallel trials. The first trial included a cohort of patients with an available, good-quality single segment great saphenous vein (SSGSV), which previous studies have shown is the optimal conduit for Bypass. As not all patients have ideal vein conduit available, the second cohort of patients compared Bypass and Endo treatment among those with only alternative conduit options. Patients in these groups were followed for an average of 2.8 and 1.9 years, respectively.
The main finding of the trial was that patients who had good quality SSGSV available and who received Bypass, had a 32 percent reduction in Major Adverse Limb Events (MALE) or death compared to Endo. This included 65 percent fewer major re-interventions and 27 percent fewer amputations. For patients who had only an alternative bypass conduit available, there was no difference in these outcome measures.
“For many patients with CLTI, clinicians may consider Endo first, but our study suggests that there shouldn’t be a one-size-fits-all approach to treatment,” said co-principal investigator Kenneth Rosenfeld, MD, Head of the Section of Vascular Medicine and Intervention in the Division of Cardiology at MGH. “What is clear from the data is that both Bypass and Endo are very effective and safe treatments, and that individualized, patient-level decision-making is very important.”
Both Bypass and Endo are considered standard-of-care treatment for patients with CLTI. For patients who receive Endo, a blockage in their artery is opened with a balloon and a wire mesh stent may be inserted permanently to maintain the opening. This procedure has become increasingly common in recent years. For Bypass, surgeons create a detour or “bypass” around the blockage in the patient’s artery by inserting a vein or a synthetic tube when an adequate vein is unavailable.
An additional important finding in the study was both Bypass or Endo revascularization reduced pain and led to significant and clinically meaningful improvements in health-related quality of life, according to the study summary. The team found that the safety, such as the number of heart attacks or strokes, and the mortality associated with the revascularization procedures being studied were similar. Taken together, the results all serve to reinforce the importance of pre-intervention assessments to help inform individualized treatment decisions for patients.
The study’s principal investigators, who represent three hospitals and two specialties, emphasized the importance of coming together from across disciplines and affiliations to help patients.
“Complex problems require interdisciplinary solutions,” said Farber. “We believe there is great value in vascular and endovascular specialists working collaboratively to identify the best treatment strategies for patients with PAD.”
Co-principal investigators are Matthew Menard, M.D.; Kenneth Rosenfield, M.D.; Taye Hamza, Ph.D.; Mark J. Cziraky, Pharm.D., FAHA; and Niteesh Choudhry, M.D., Ph.D. Authors’ disclosures are listed in the abstract. The study was funded initially by the National Heart, Lung, and Blood Institute, a division of the National Institutes of Health. Funding during the follow-up period (2019-2021) was provided by Vascular InterVentional Advances (VIVA), the Society for Vascular Surgery, the New England Society for Vascular Surgery, the Western Vascular Society, the Eastern Vascular Society, the Midwest Vascular Surgery Society, the Southern Association of Vascular Surgeons, the Canadian Society for Vascular Surgery, the Society for Clinical Vascular Surgery, the Society of Interventional Radiology, the Vascular and Endovascular Surgery Society, the Society for Vascular Medicine; Janssen; Gore; Becton Dickinson and Company; Medtronic; Cook; Boston Scientific; Abbott; Cordis; and Cardiovascular Systems, Inc.
The team has additional analyses planned from the treasure trove of data that has been generated by the BEST-CLI trial (Number NCT02060630). Menard, Farber and Rosenfield recently received further funding from the Novo Nordisk Foundation to extend and amplify their initial analysis, noted the trial summary by the Boston University Chobanian & Avedisian School of Medicine.
For more information: https://professional.heart.org/en/meetings/scientific-sessions/science-news-for-2022


 November 14, 2025
November 14, 2025